Cranialization
Preoperative Considerations
Consent:
- Hair los
- Cosmetic changes
- Infection
- Tissue death if avulsive injury & closed under tension
- Muccele formation if incomplete removal of sinus lining
Anesthesia/Positioning:
- Supine
- Mayfield headrest
Other:
- None
Armamentarium:
- Skin prep
- Marking pen
- Local anesthesia
- Cranial drape
- #10 blade
- Monopolar and bipolar electrocautery
- Raney clips
- Curved hemostat and Kelly hemostat
- Periosteal elevators
- Cranial drill and protected blade (PRN)
- Mesh (PRN) and plating system with mono-cortical fixation
- Adison pickups
- Suture scissors
- Flat JP drain with bulb and drain suture (2-0 nylon)
- 2-0 vicryl
- Skin stapler
- Bacitracin
- Non-adherent dressing (Telfa, etc)
Technique






























Postoperative Considerations
Immediate:
- Q4 drain maintenance - remove after producing <30 cc/day
- No baths or still bodies of water until incision sites fully heald
- Consider H&H if excessive blood loss
Follow Up:
- Remove staples approximately 10 days post op. Every other staple if slow healing.
- Monitor for wound dehiscence
- Monitor for signs of infection
Operative Note
Surgeon(s): ***
Assistant Surgeon(s): ***
Preoperative Diagnosis: ***
Postoperative Diagnosis: Same
Procedure(s): ***
Anesthesia: General
Implants: None
Specimen:***
Drains: None
Fluids: See anesthesia record
EBL: Minimal
Complications: None
Counts: Correct x2
Indications: ***
Findings: As expected
Procedure in Detail:
The patient was seen in the preoperative holding area with a H&P was updated, consents were verified, surgical site marked, and all questions and concerns related to the proposed procedure were discussed in detail. The patient was transferred to the operating room by the anesthesia team. The patient underwent general anesthesia with endotracheal intubation. Tegaderms were placed over the eyes. The patient was prepped and draped in the standard fashion for maxillofacial procedures. A time-out was performed and the procedure began.
Hair was parted with ultrasound jelly and the incision site was marked in an M shaped pattern with cross hatch marks at the midline and on the lateral portions of the incision. 10 cc of of 2% lidocaine with 1:100k epinephrine was injectedt the marked incision site.
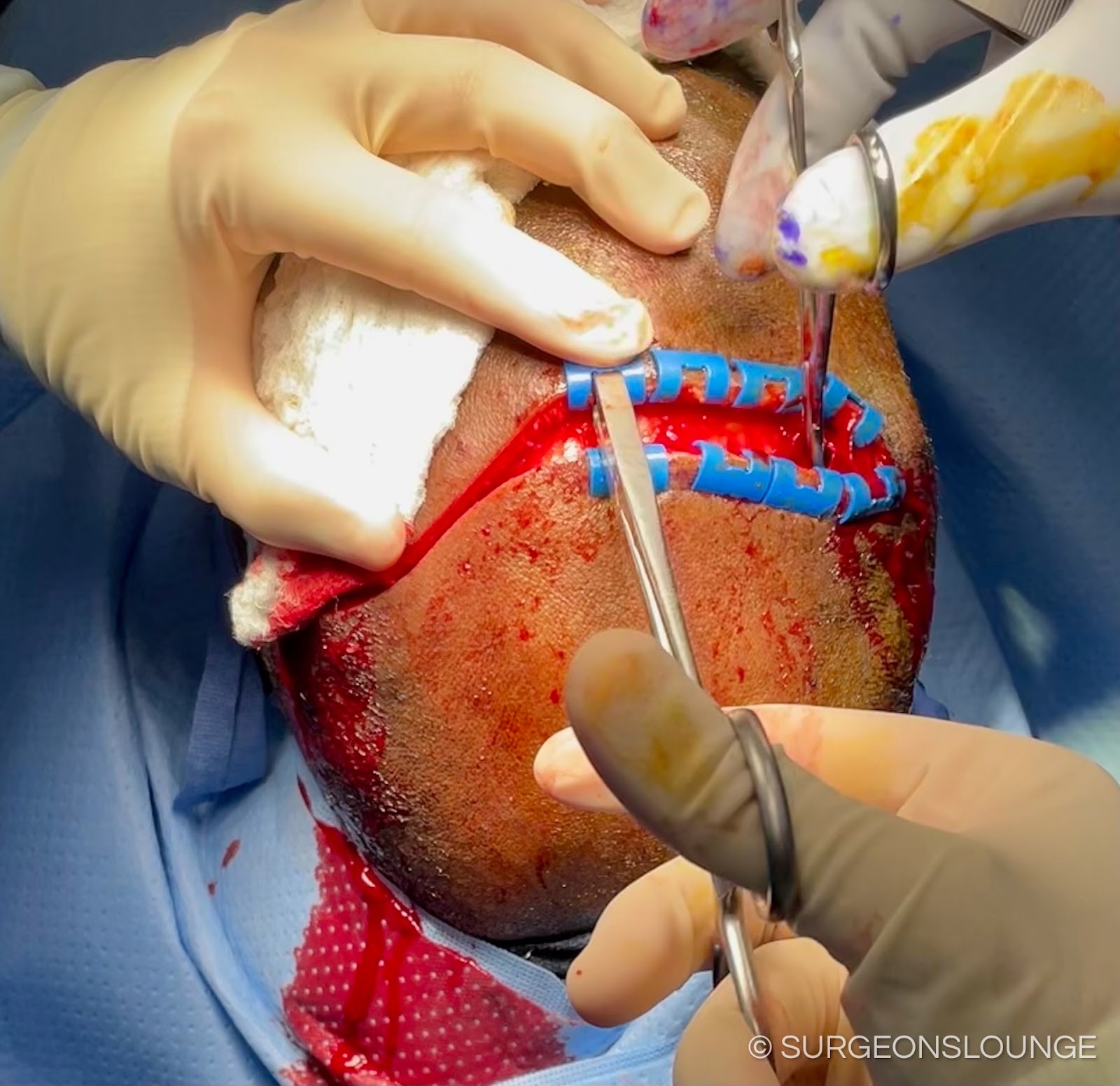
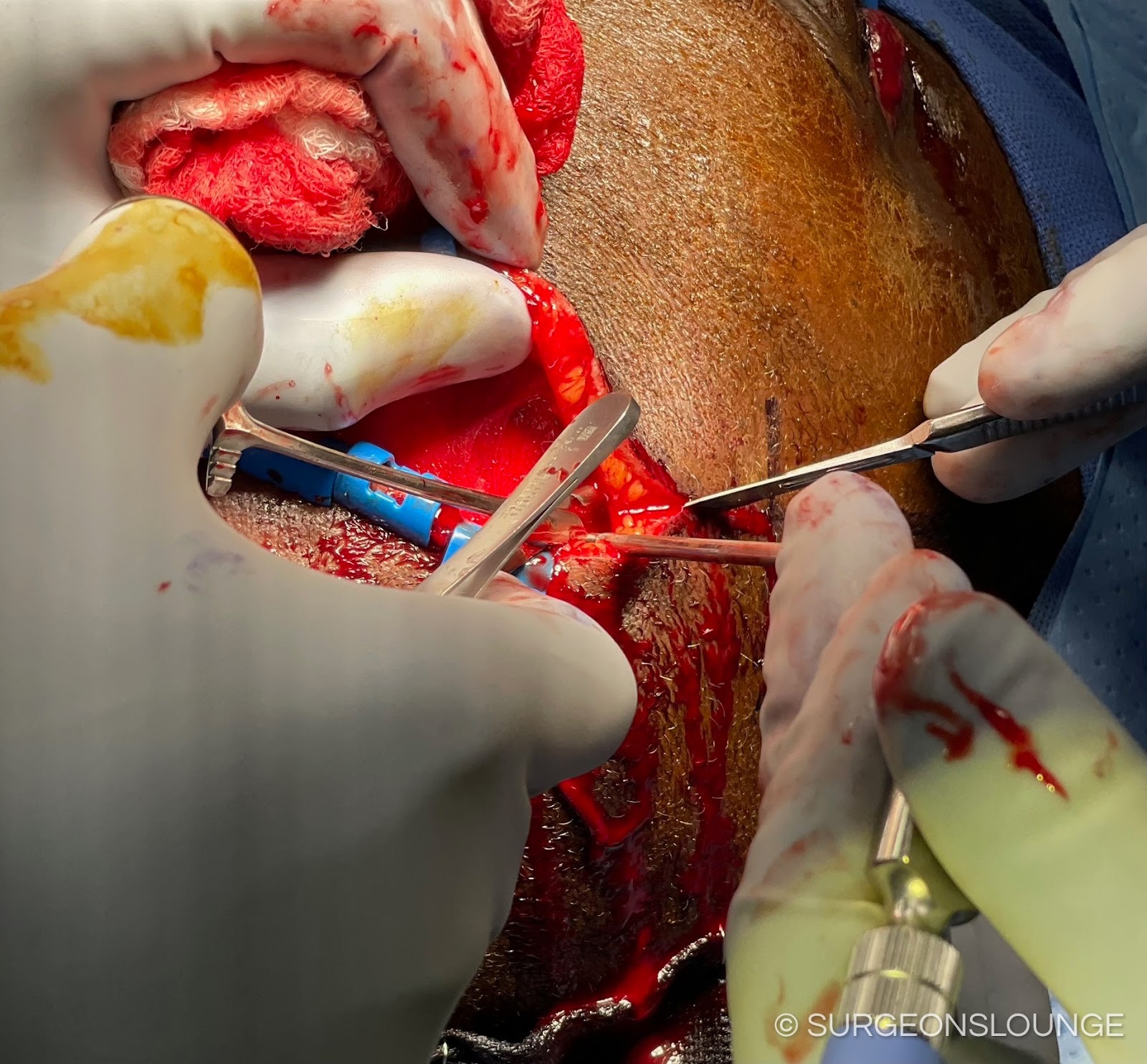
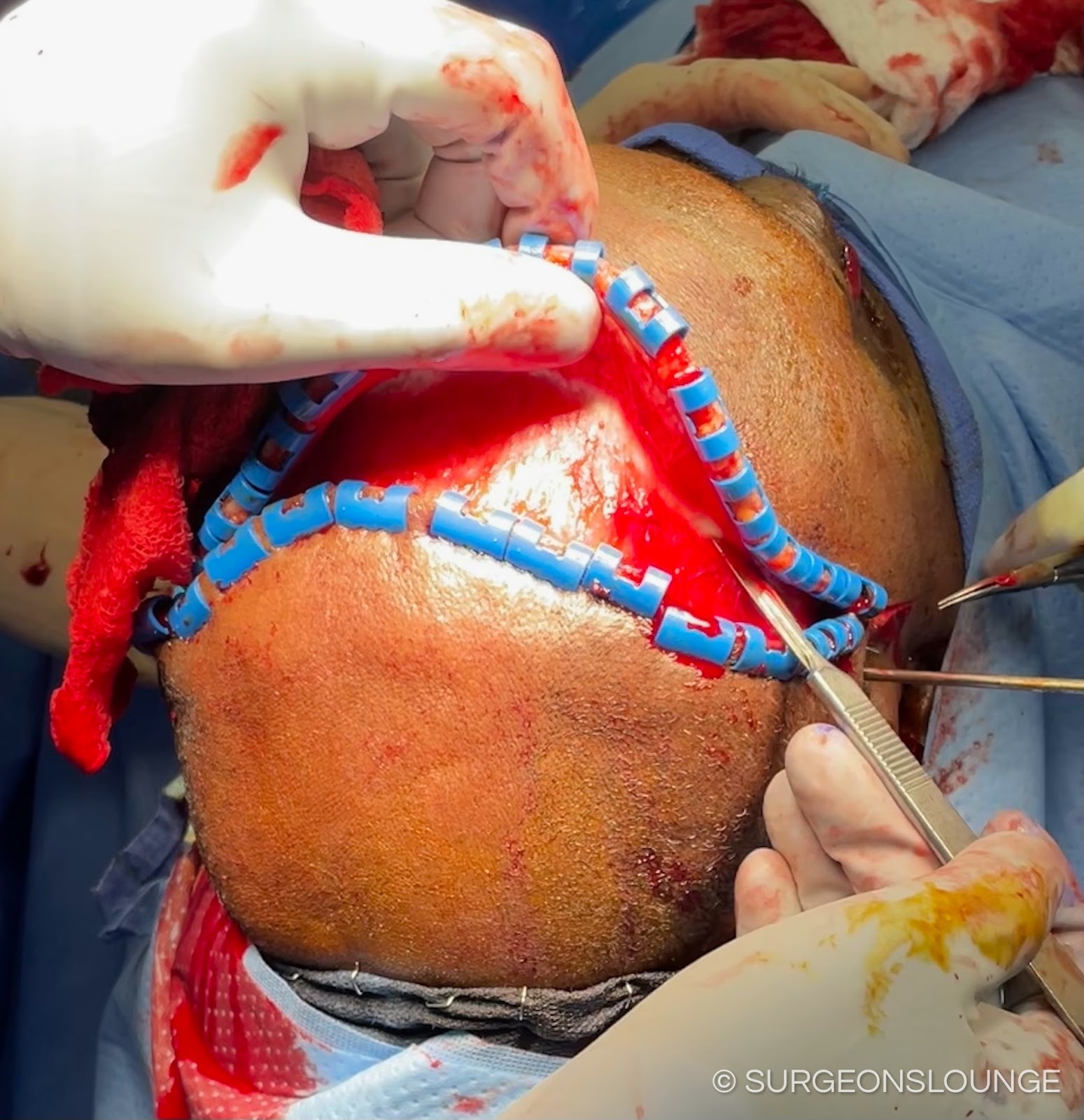
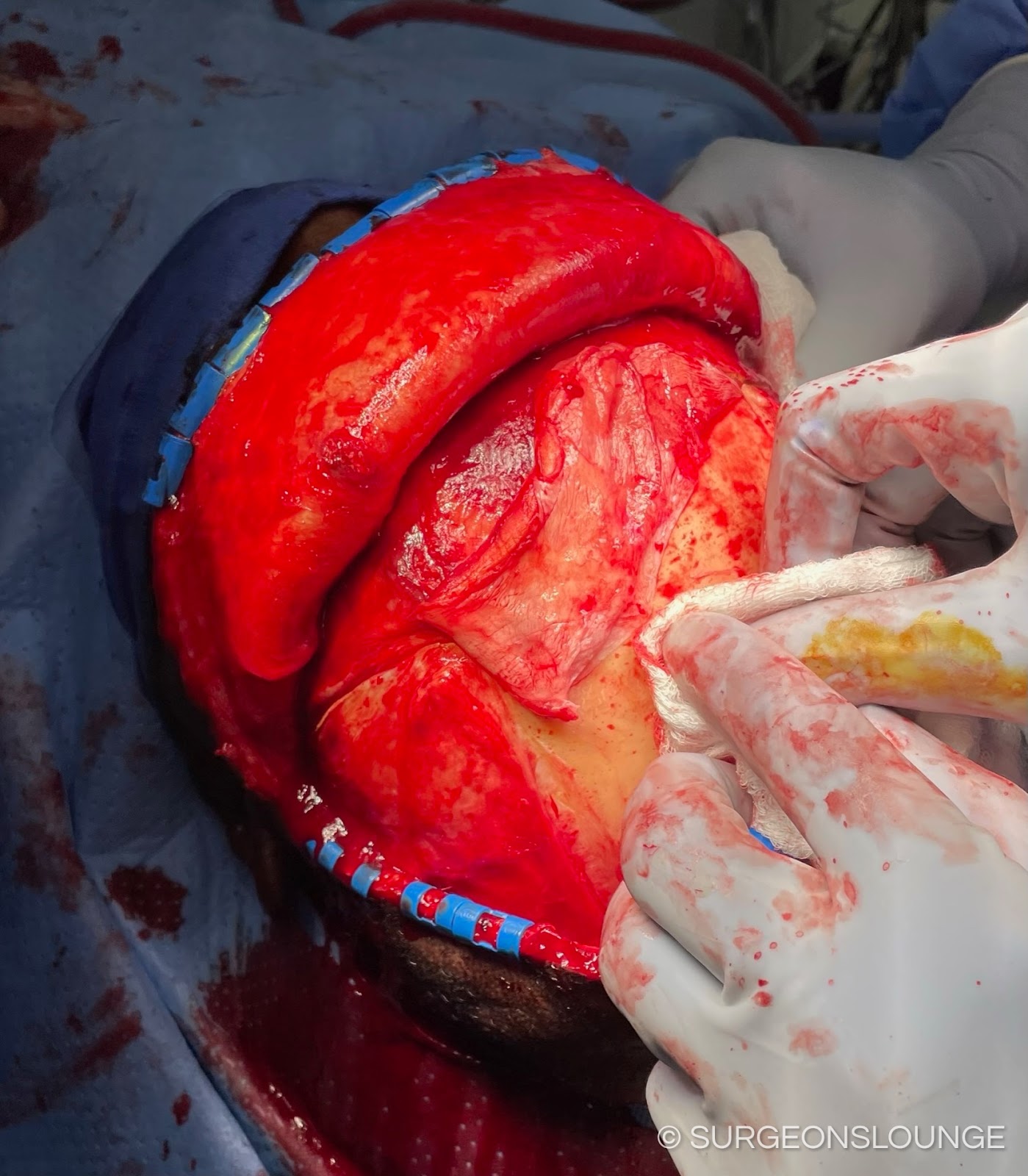
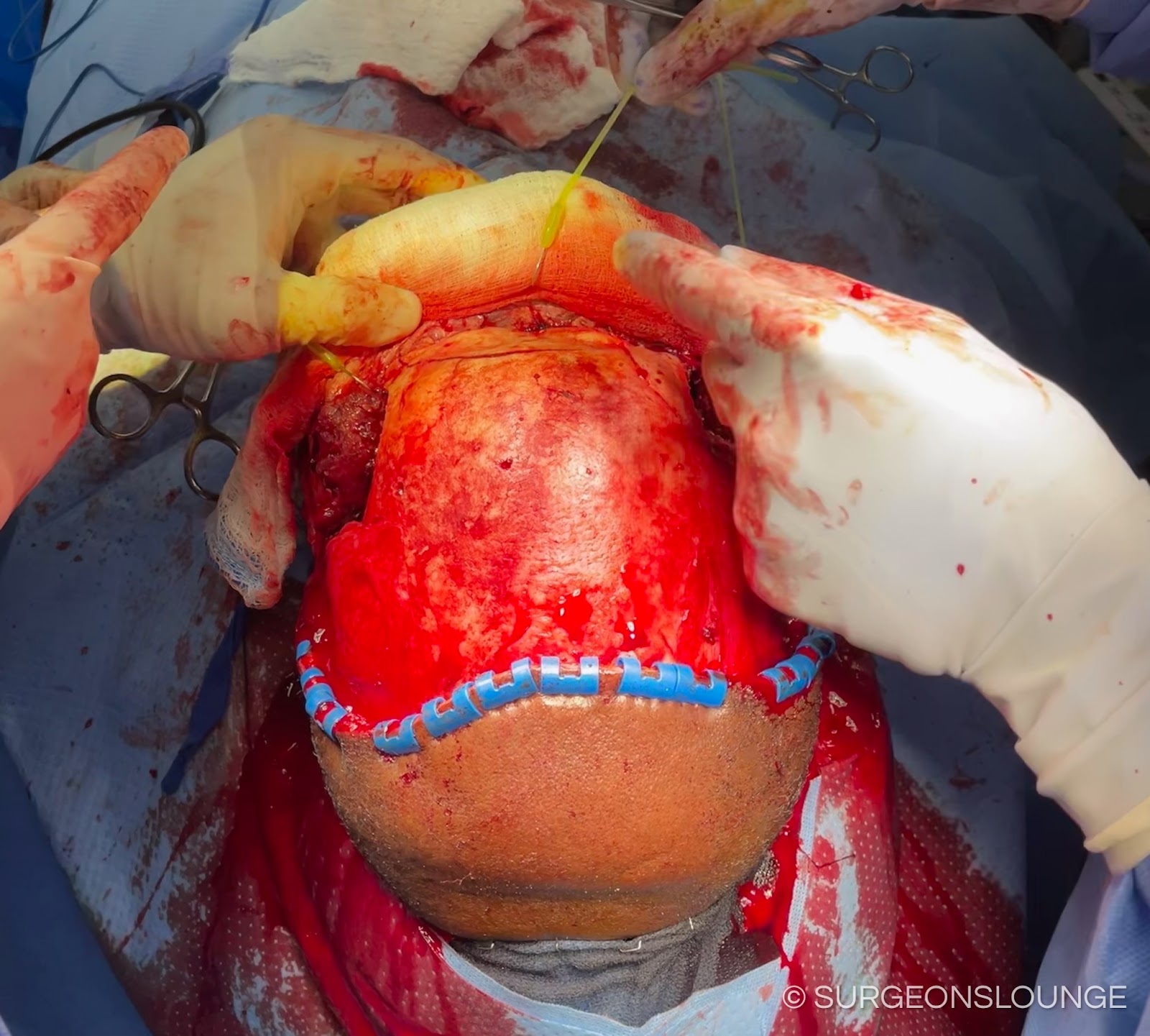
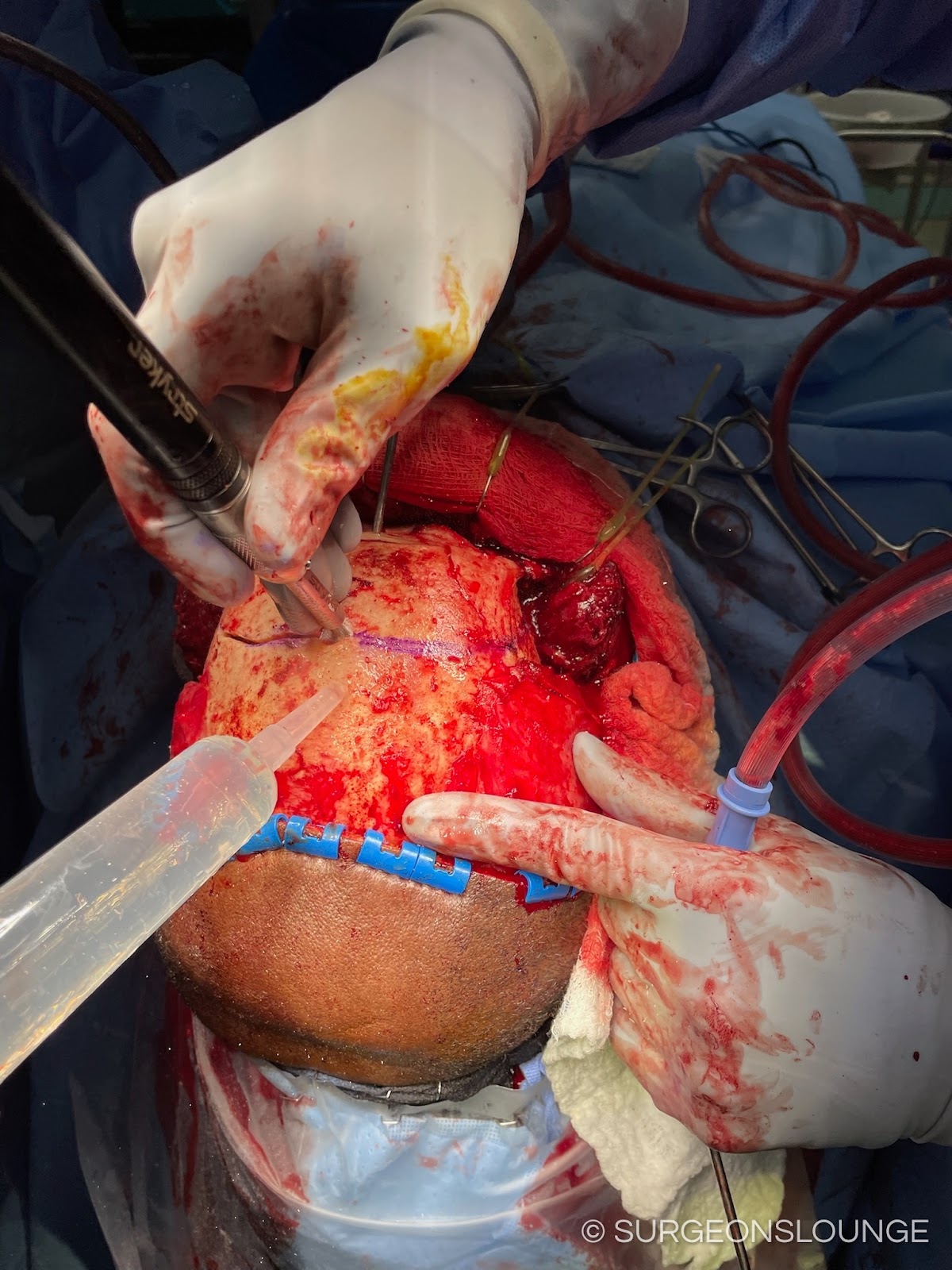
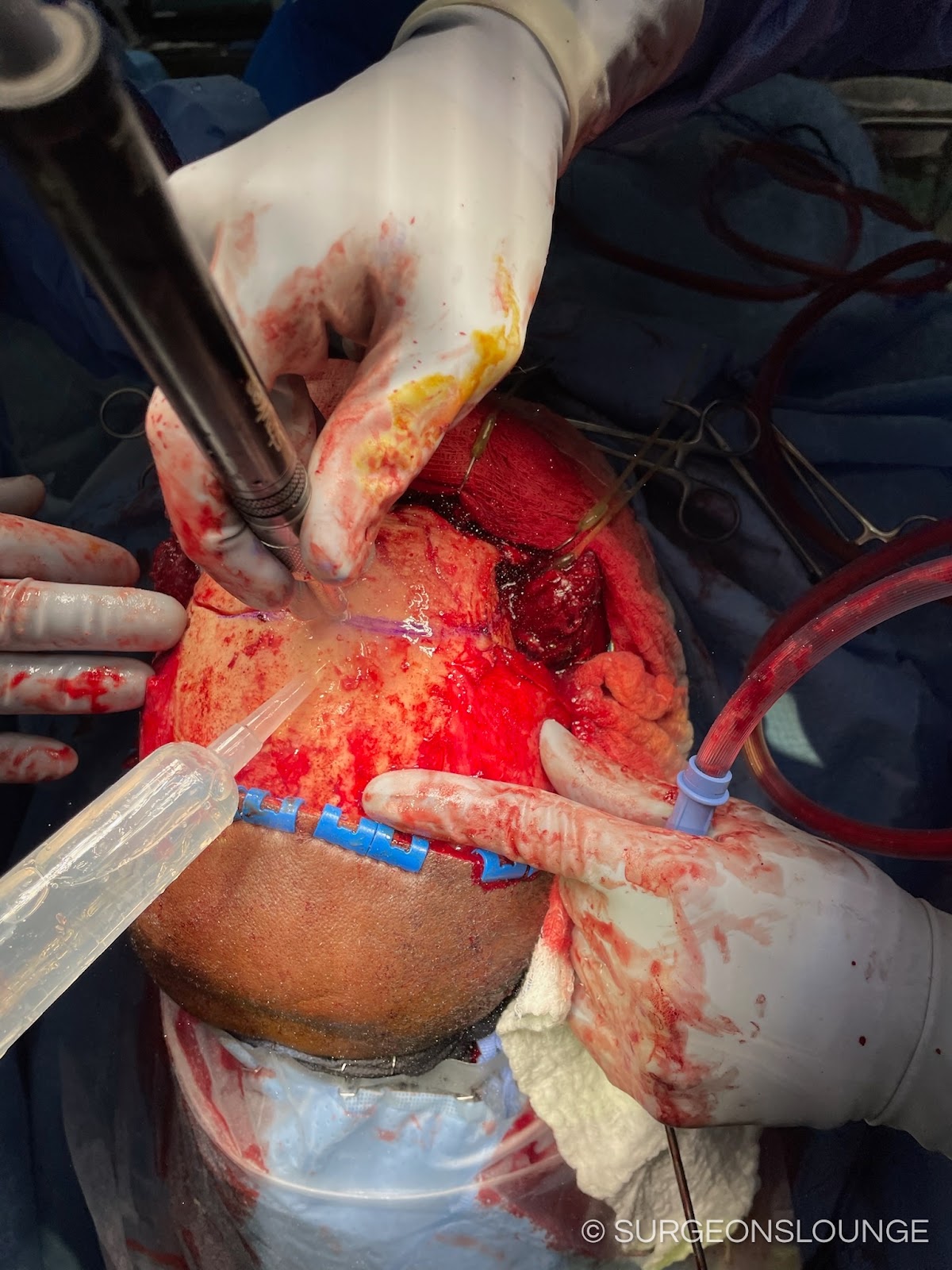
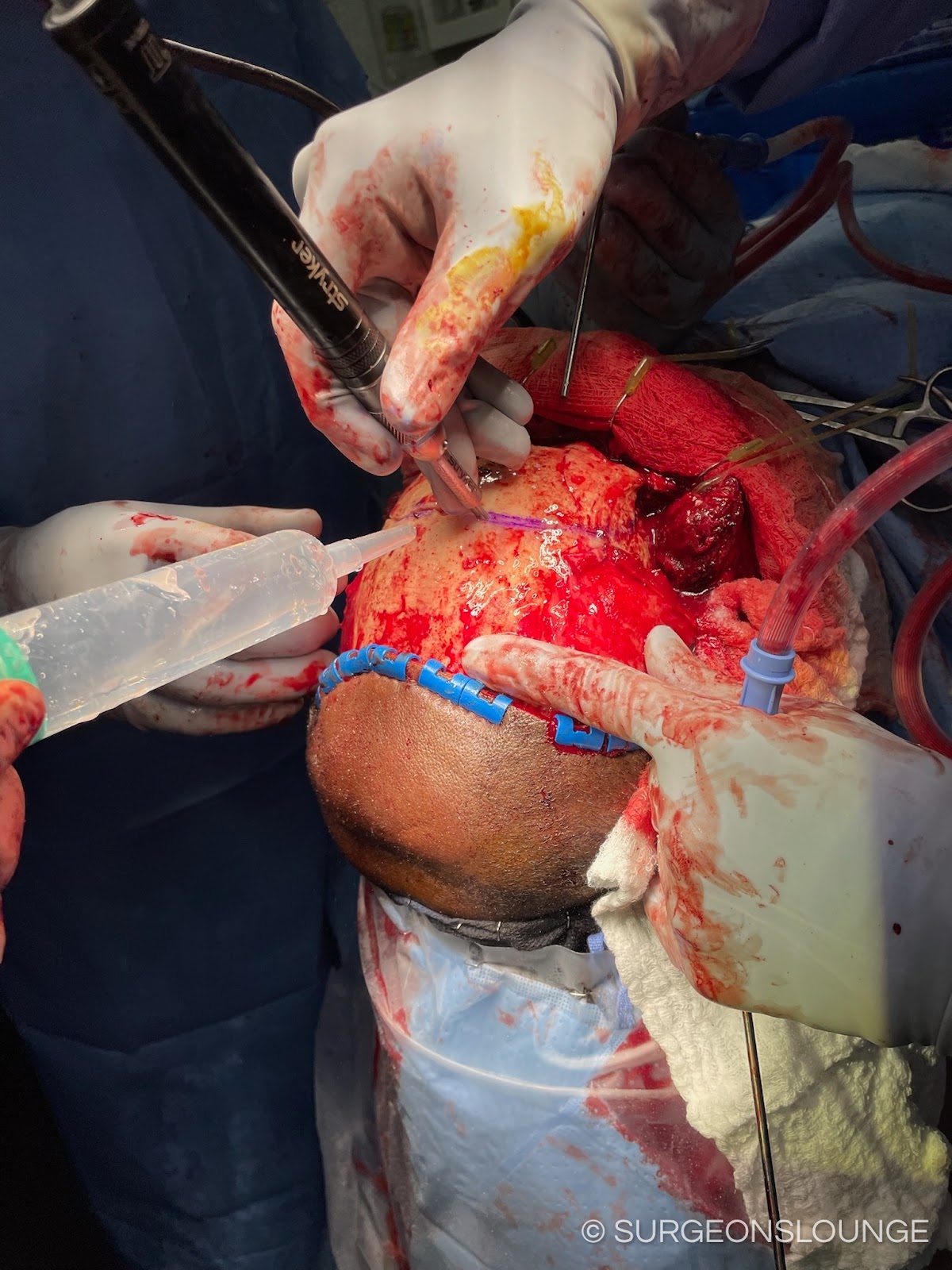
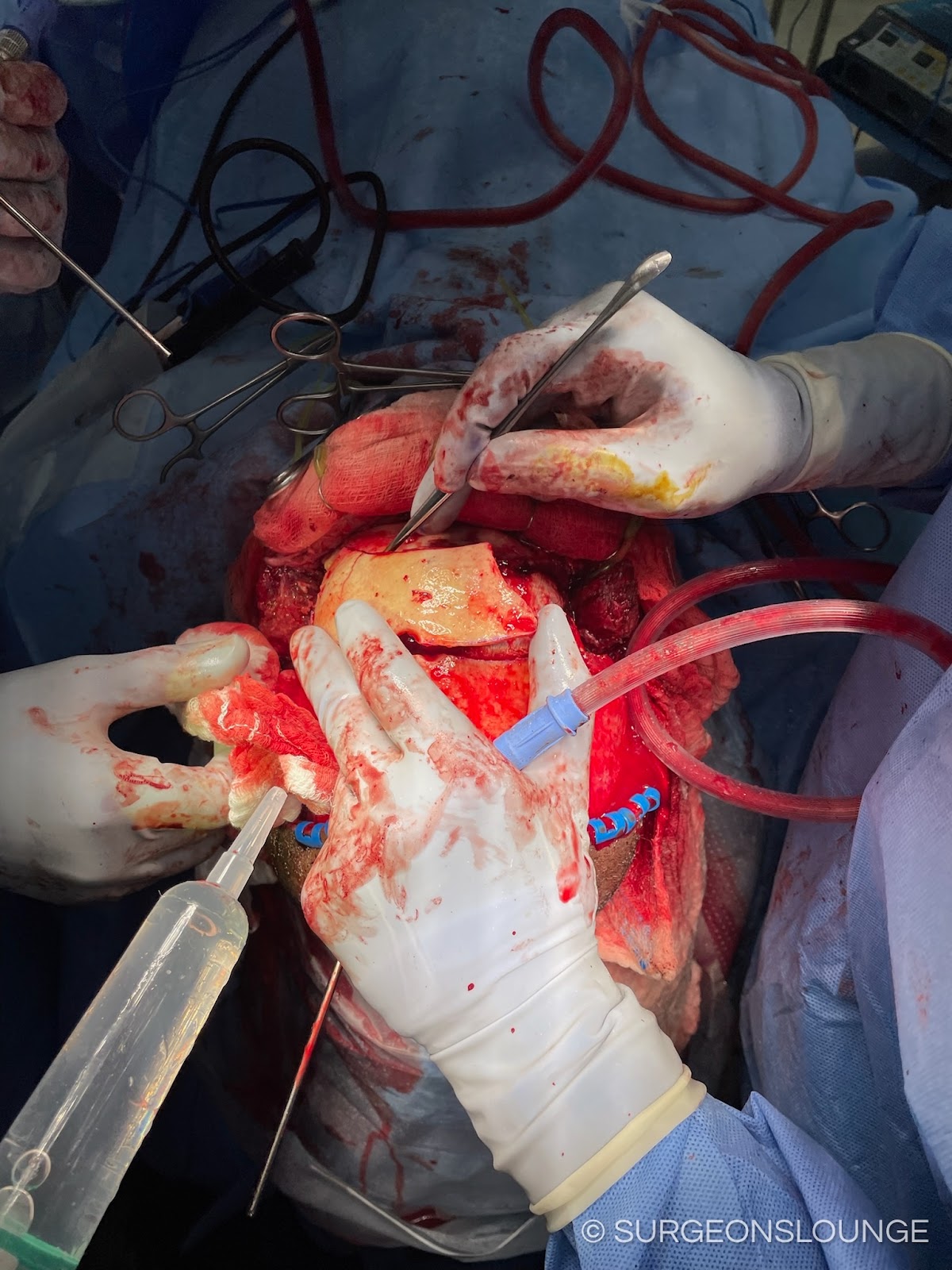
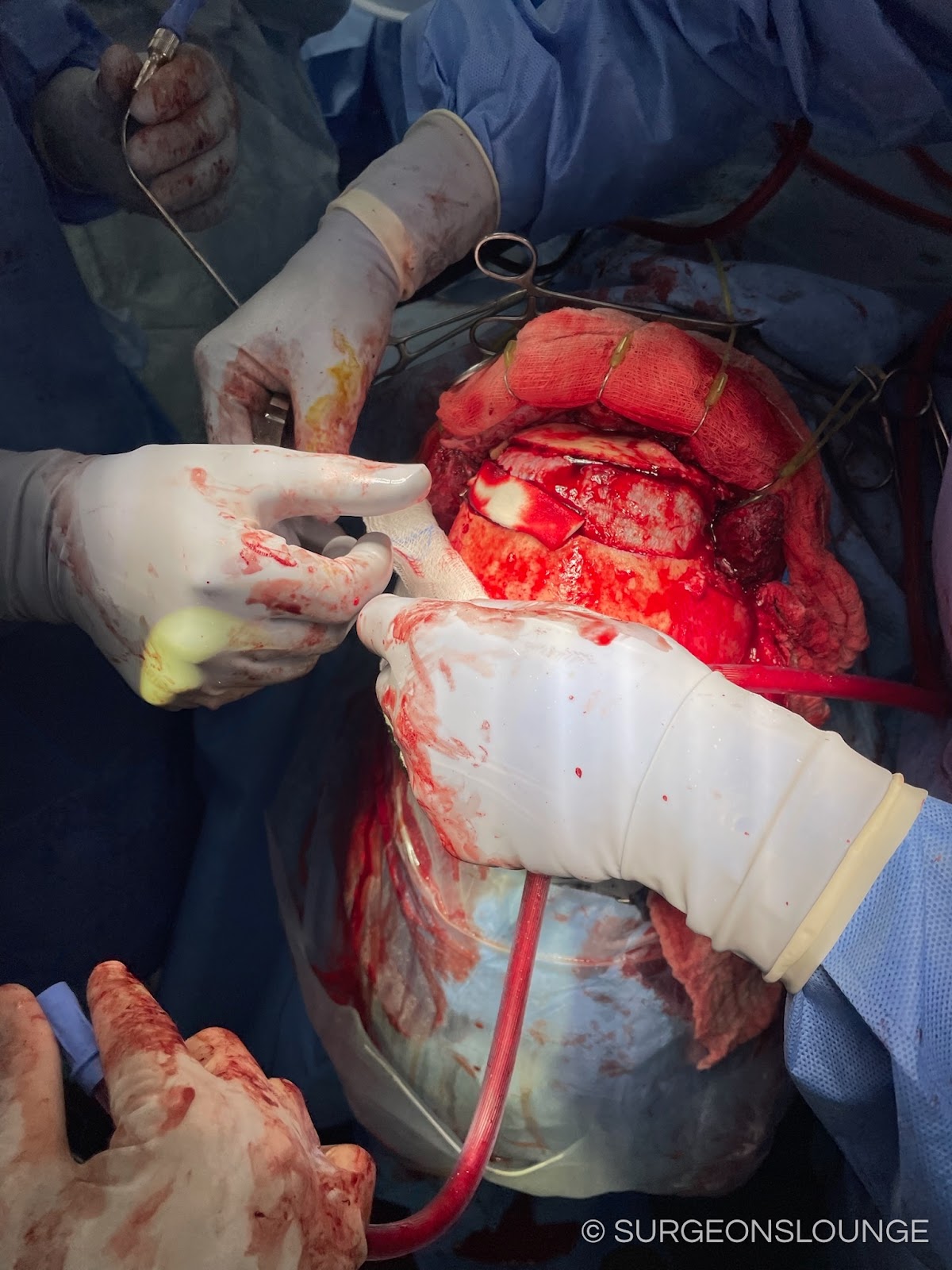
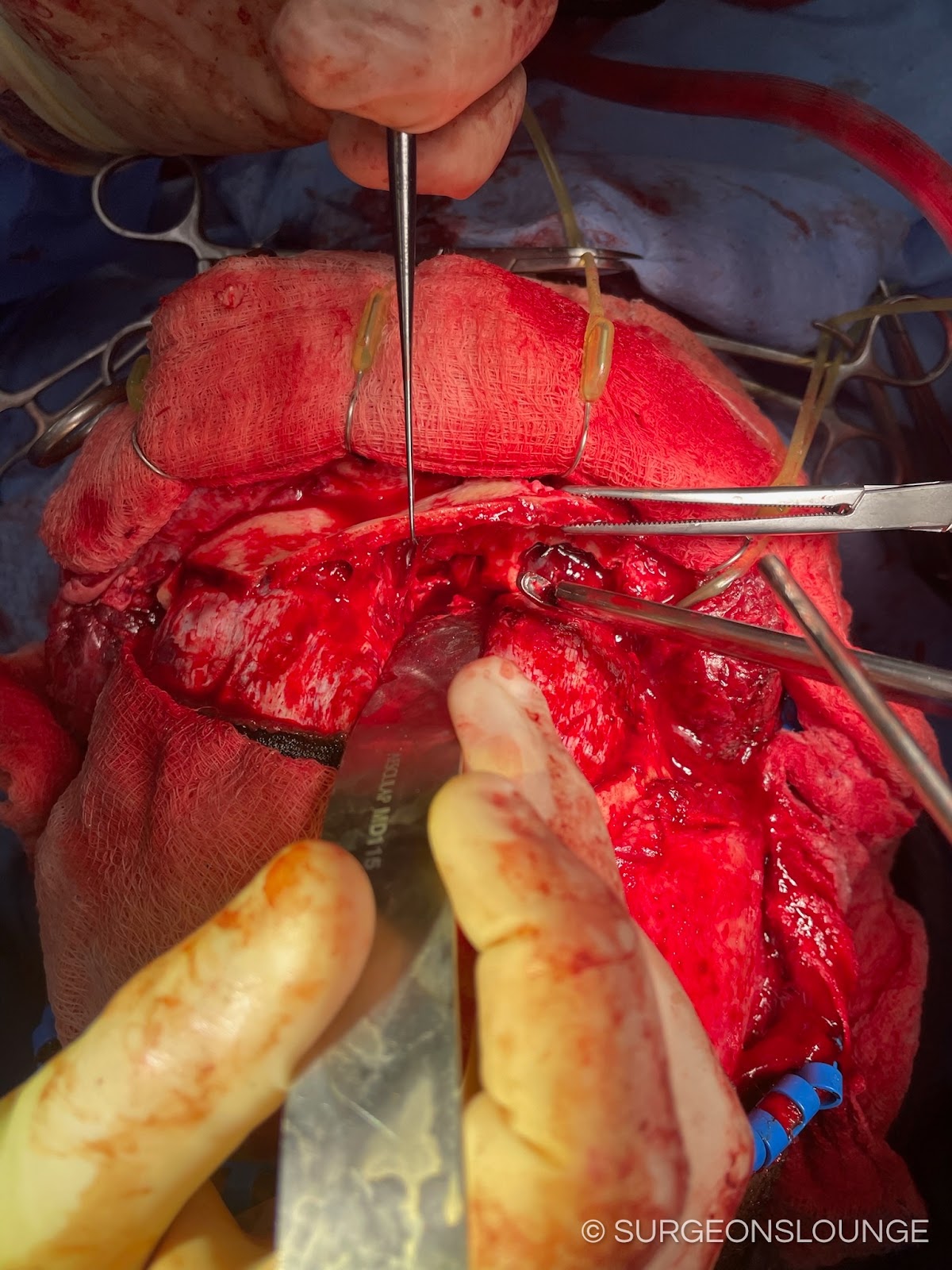
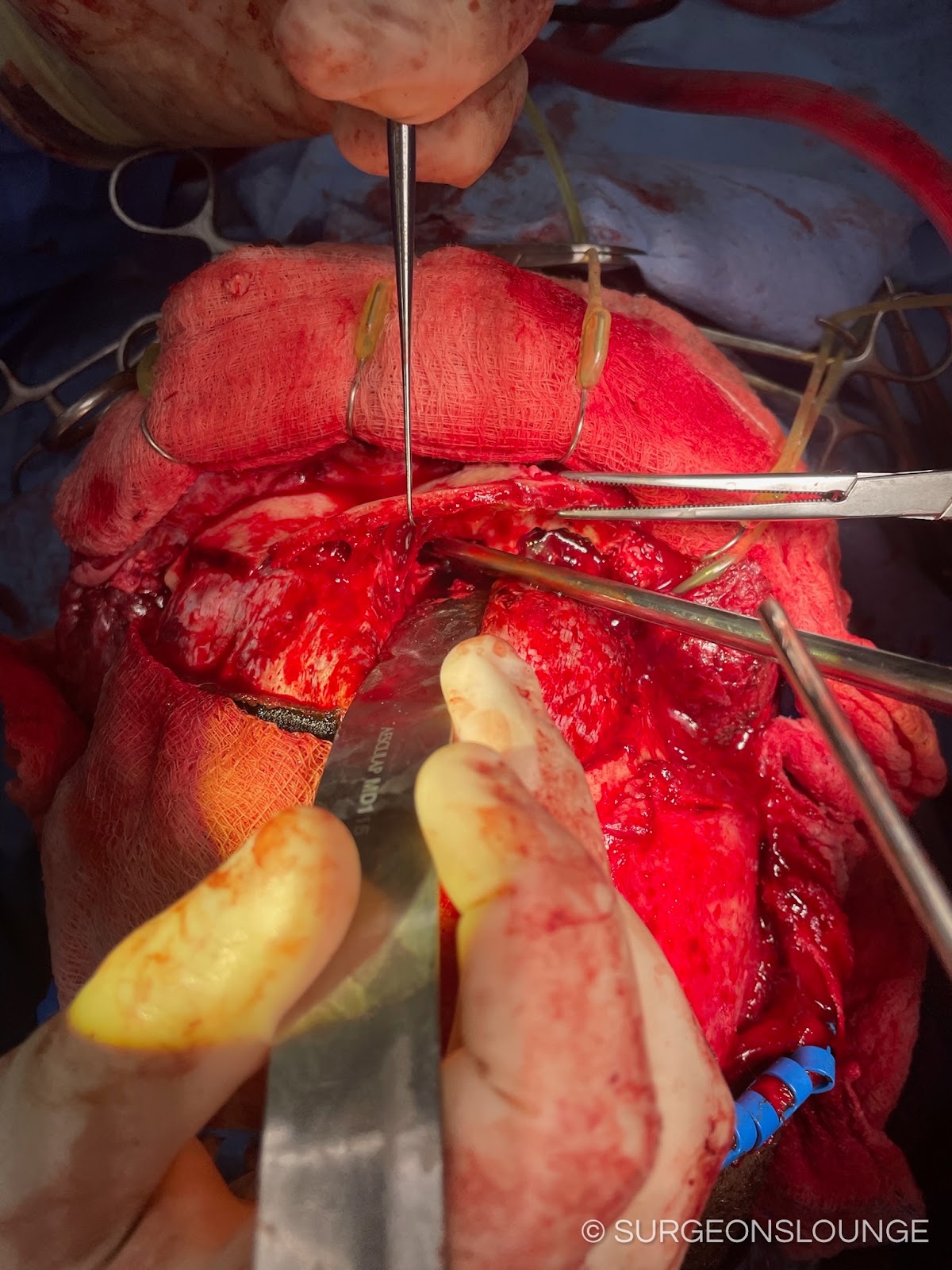
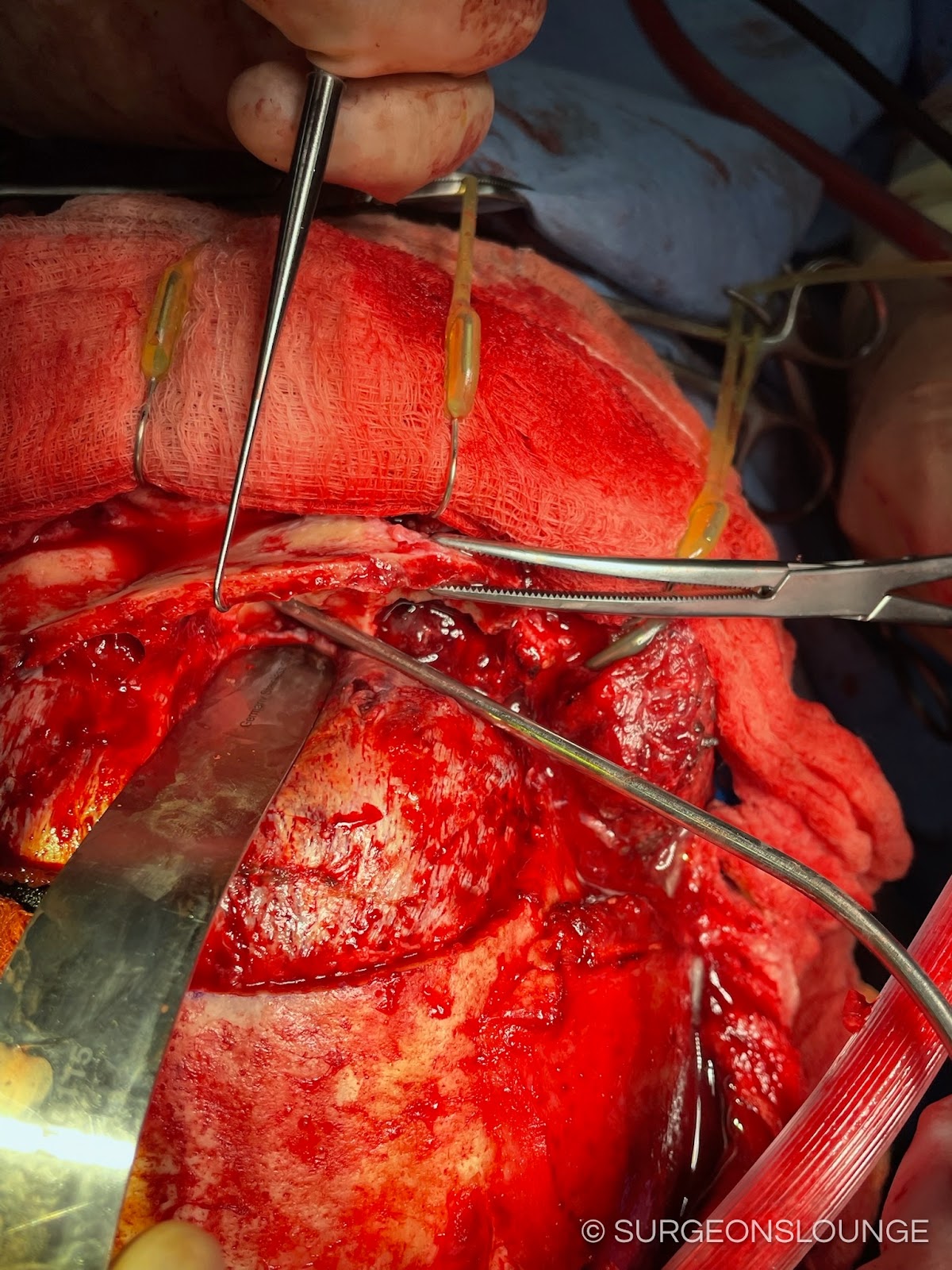
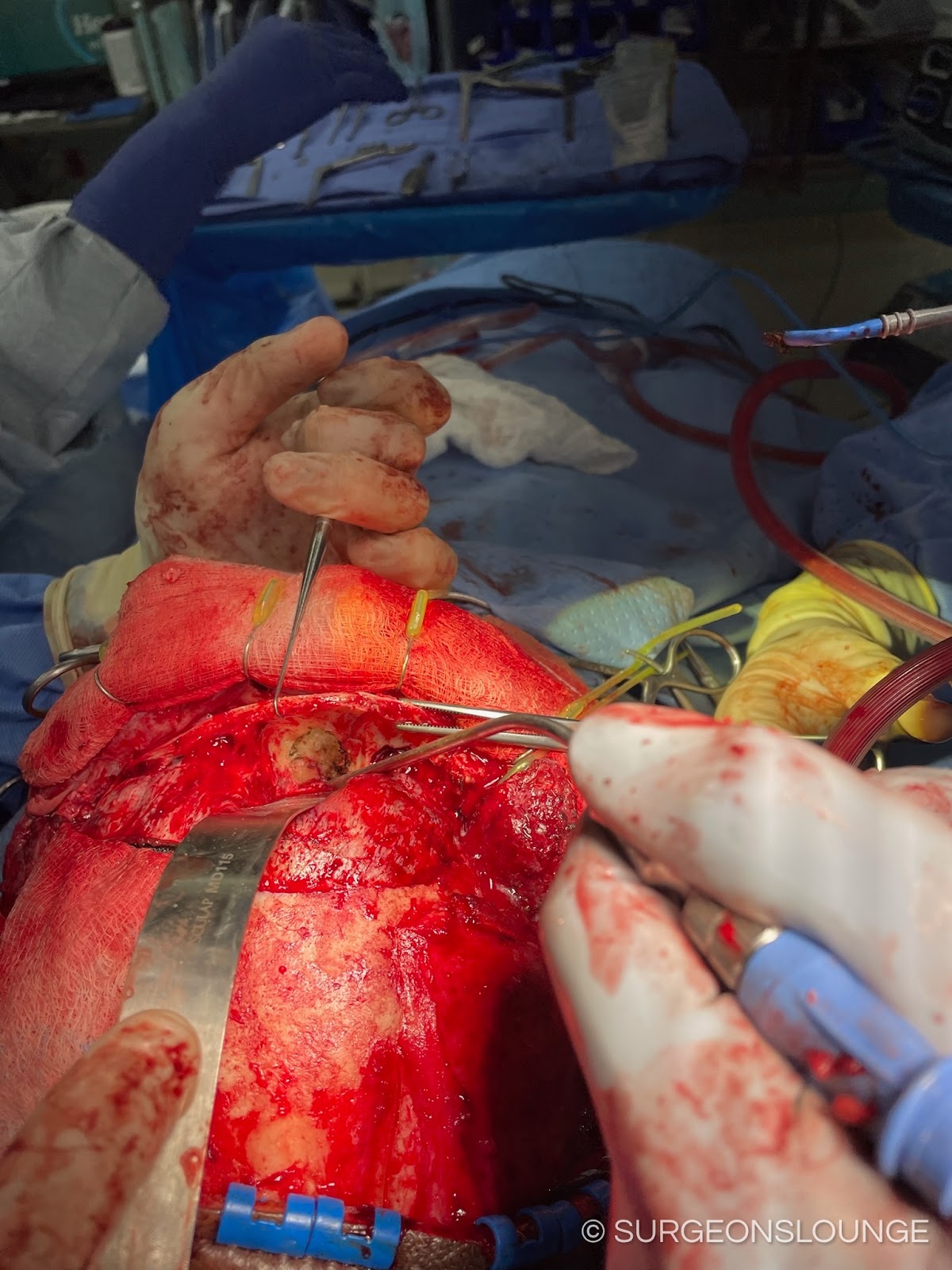
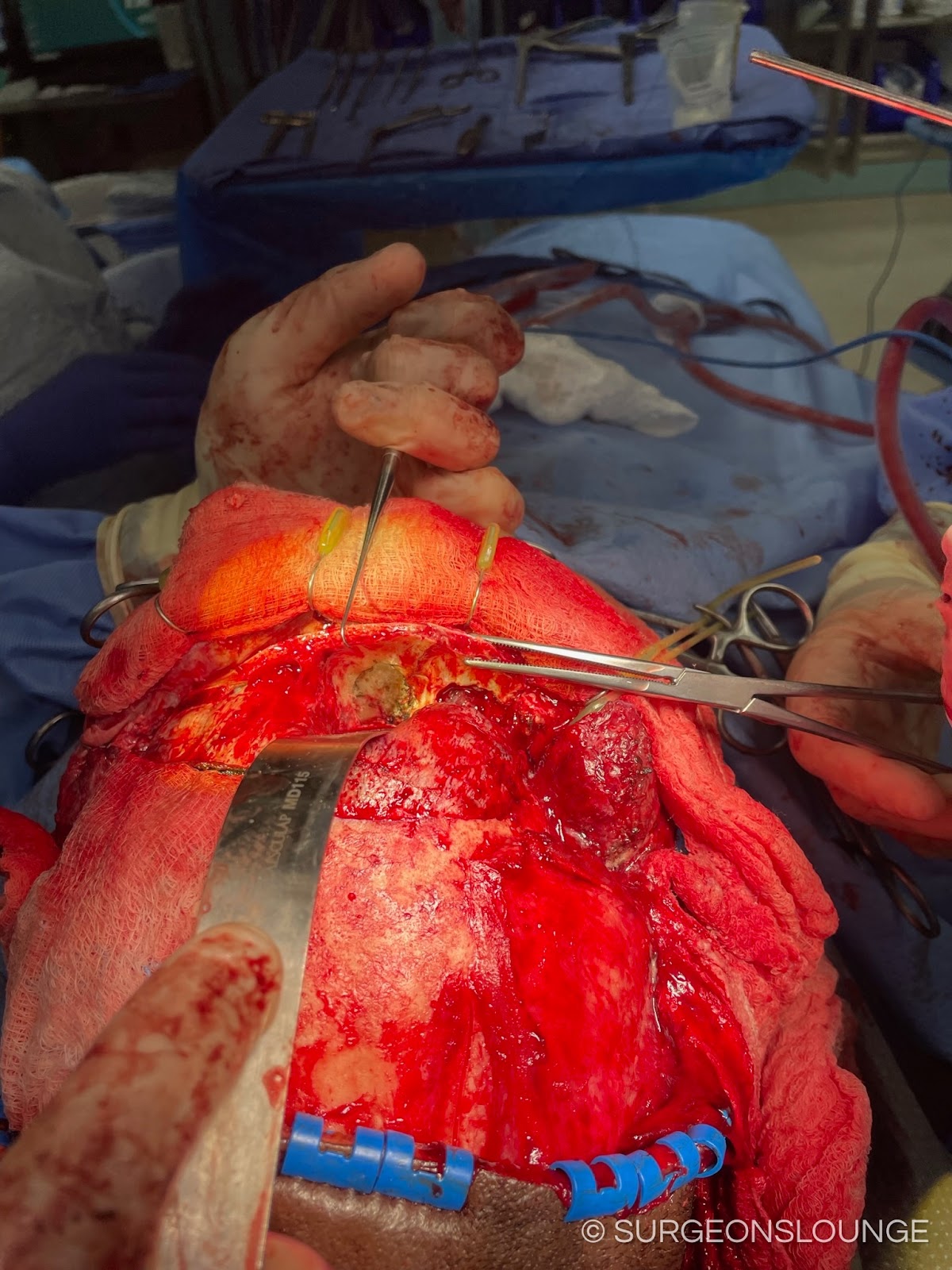
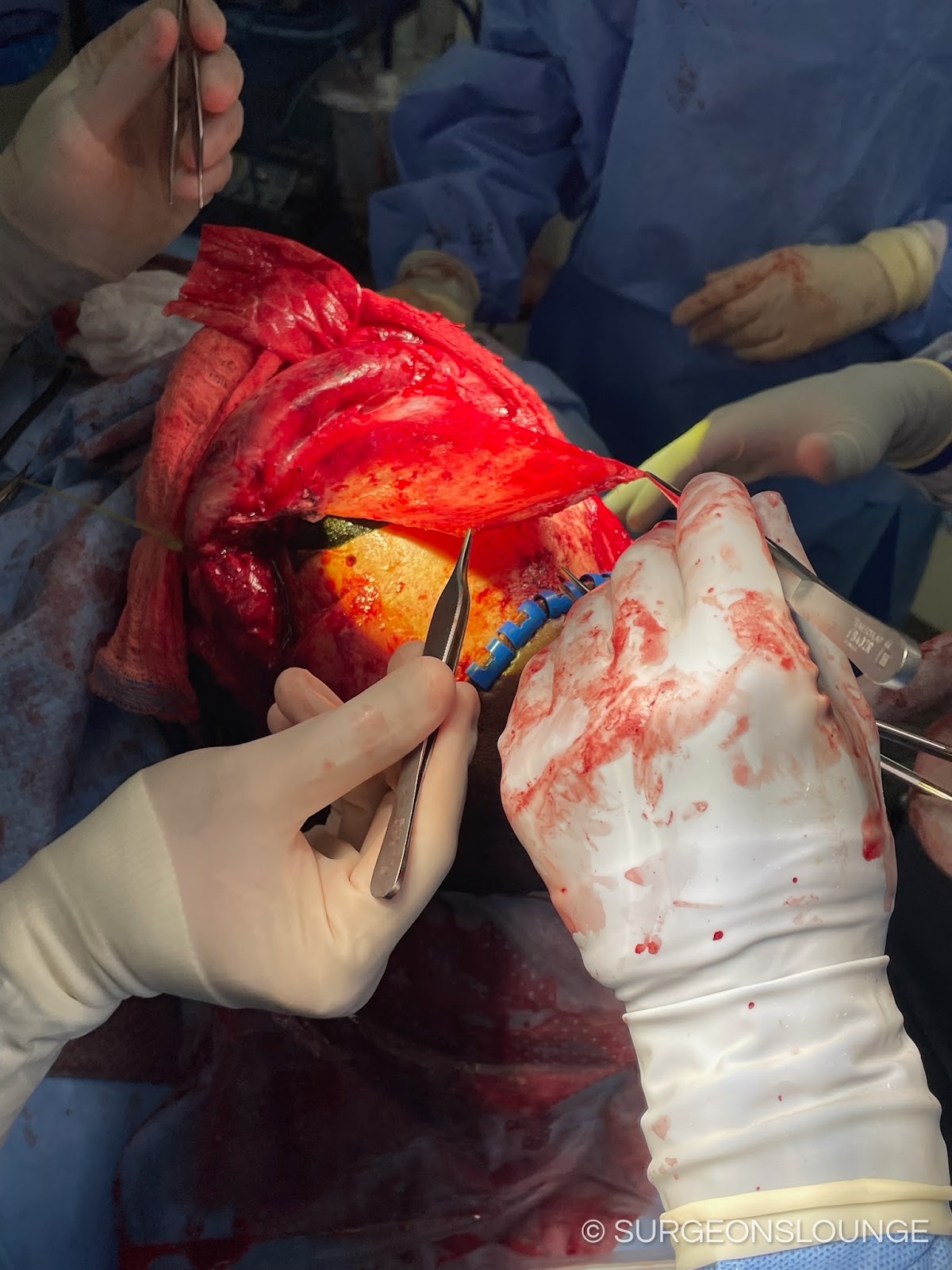
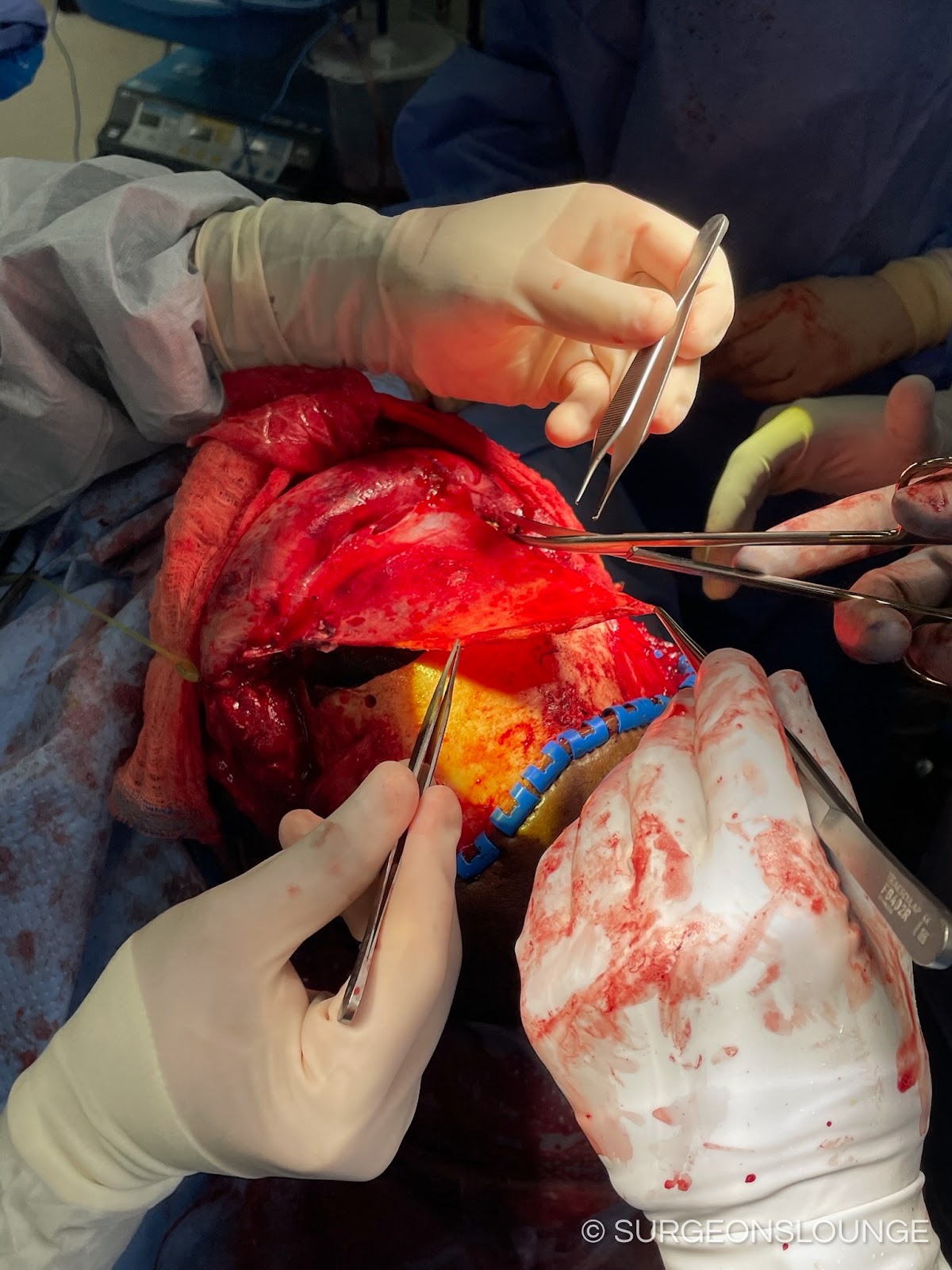
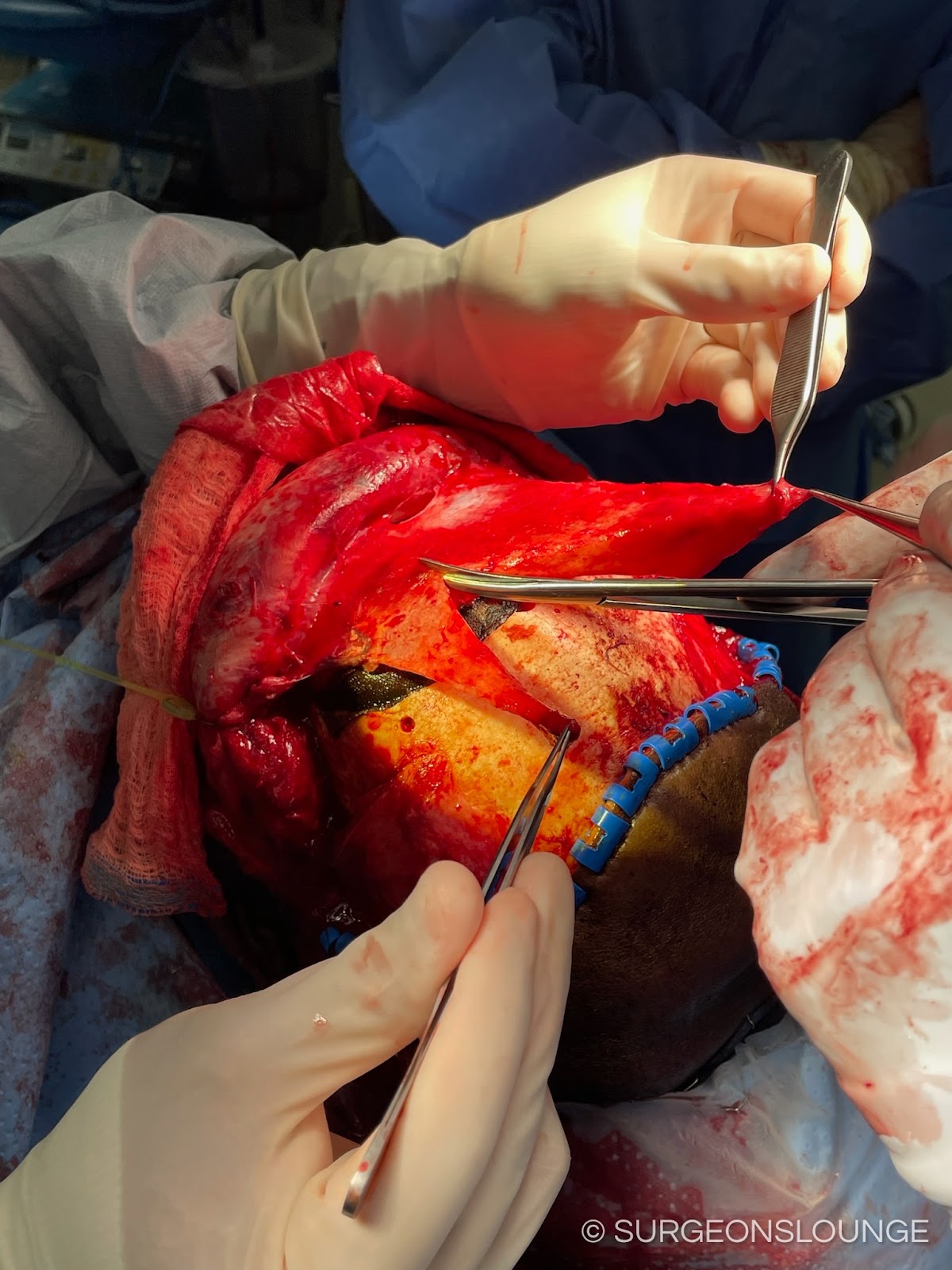
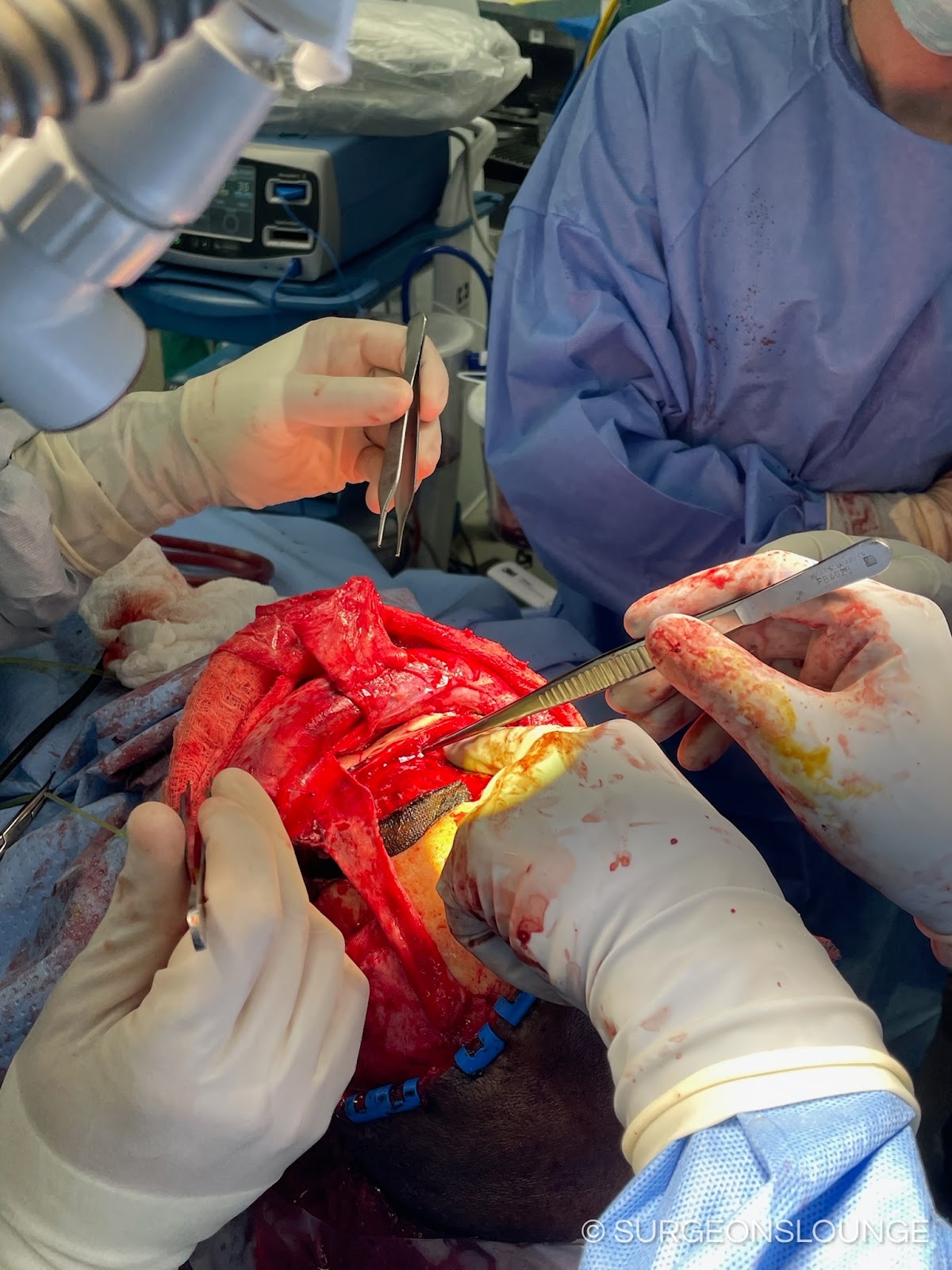
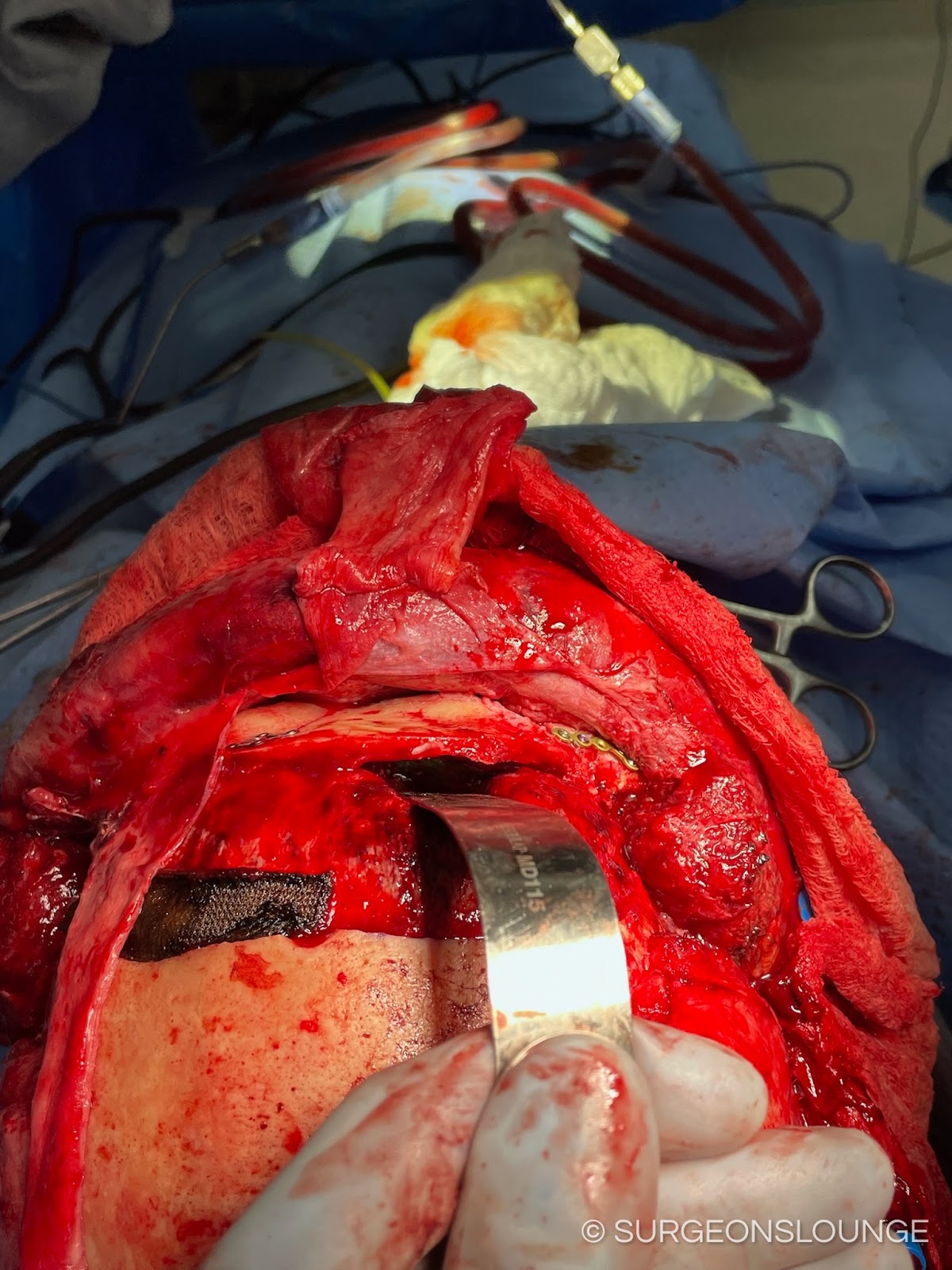
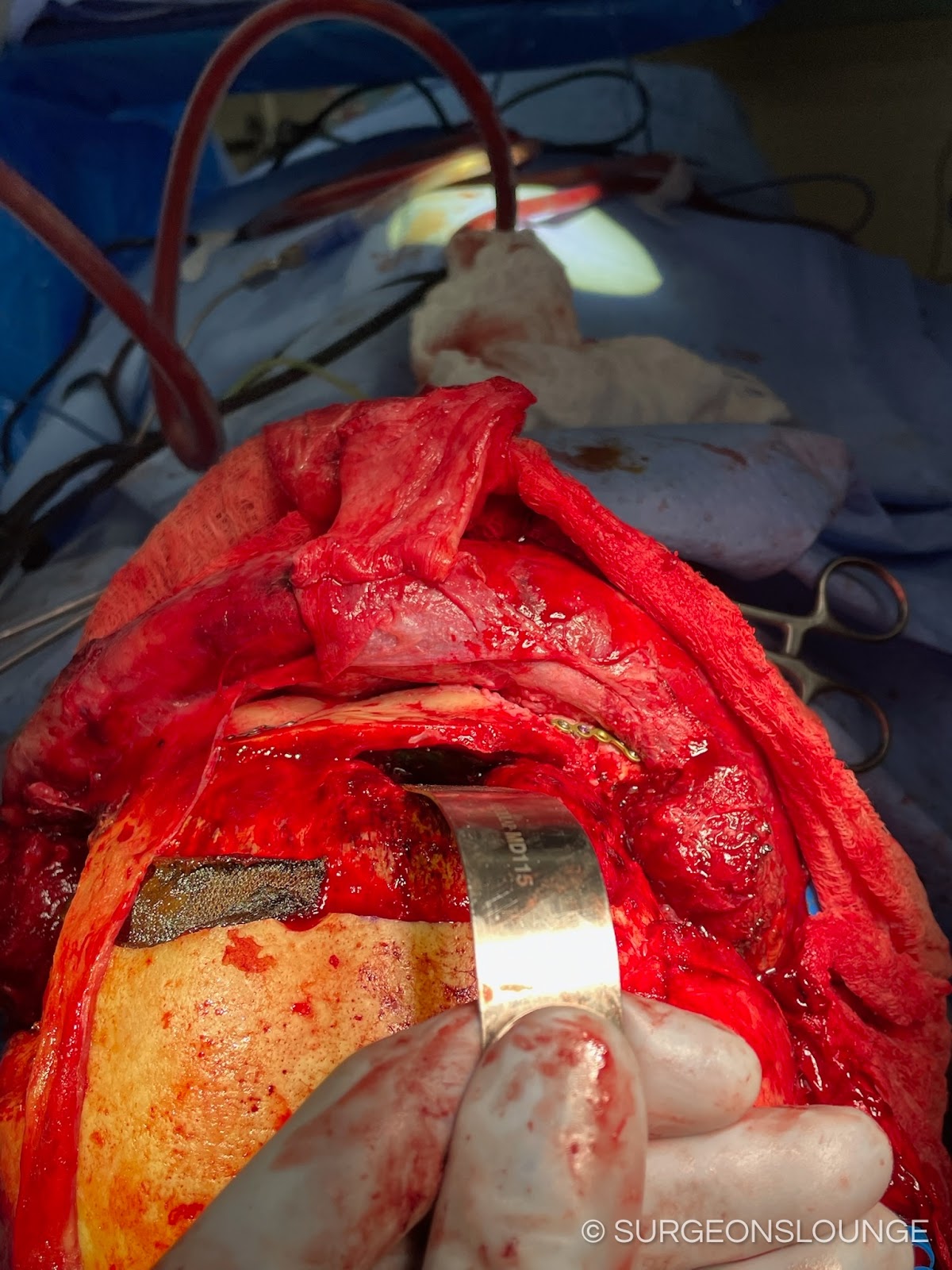
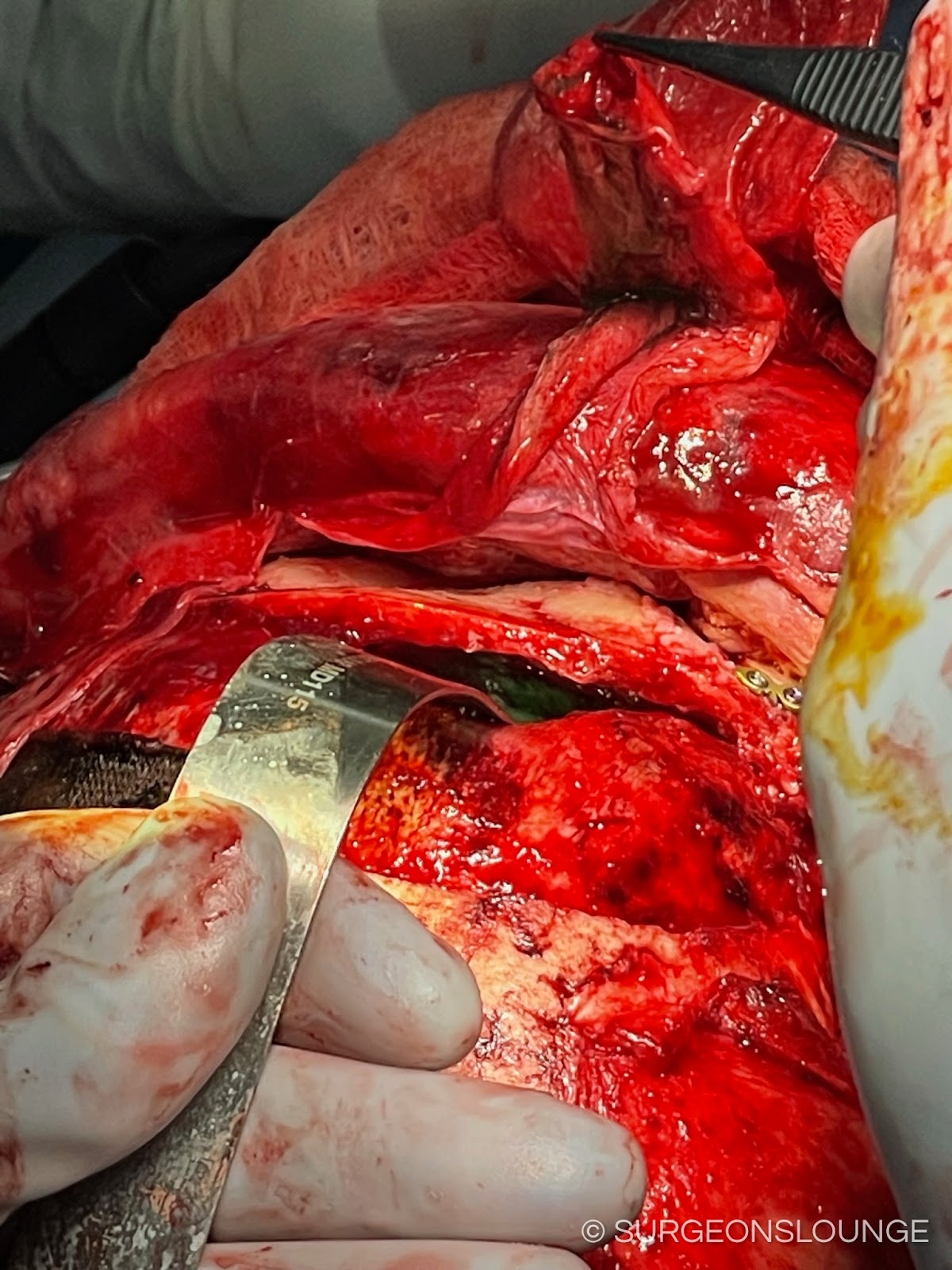
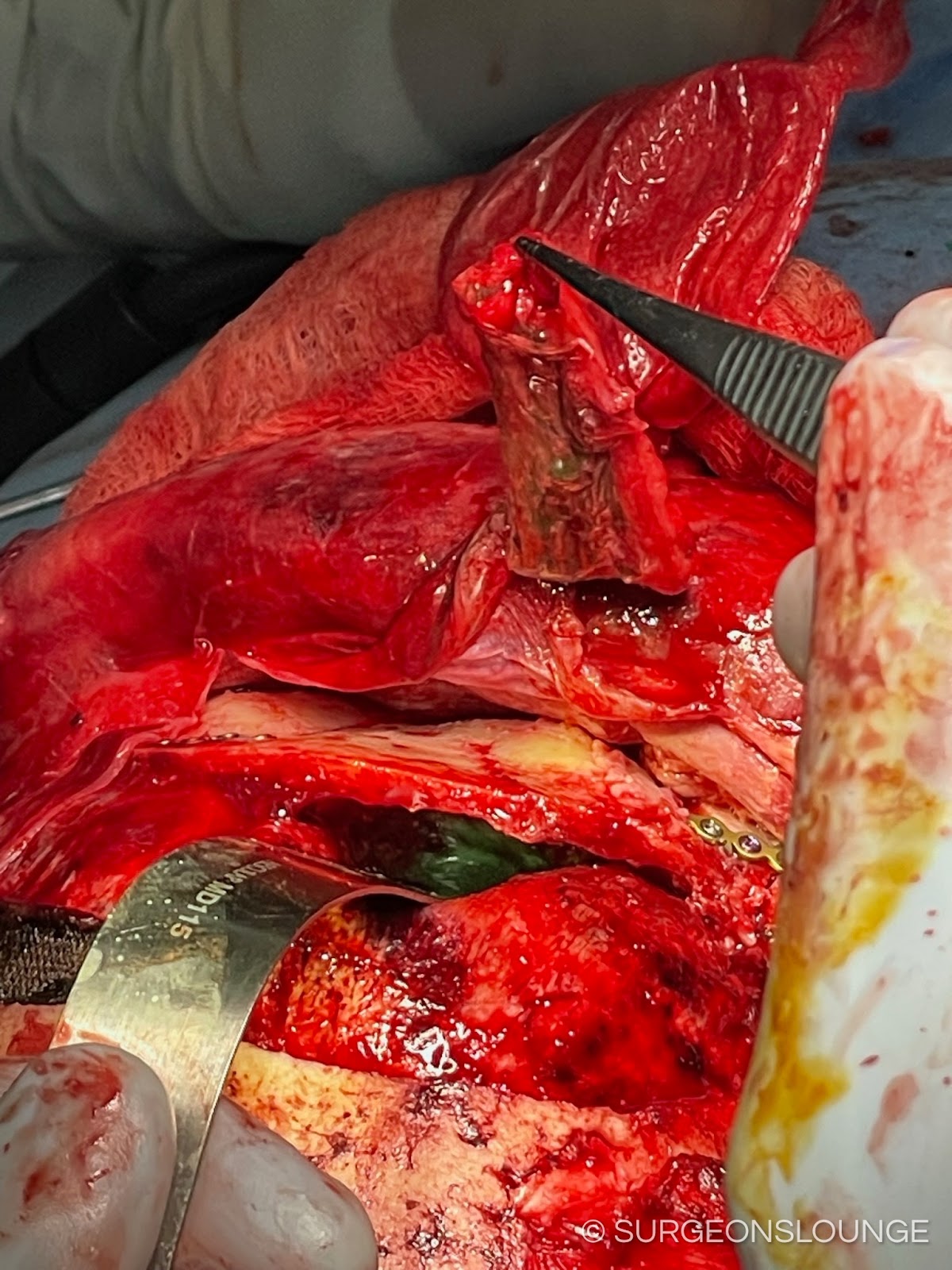
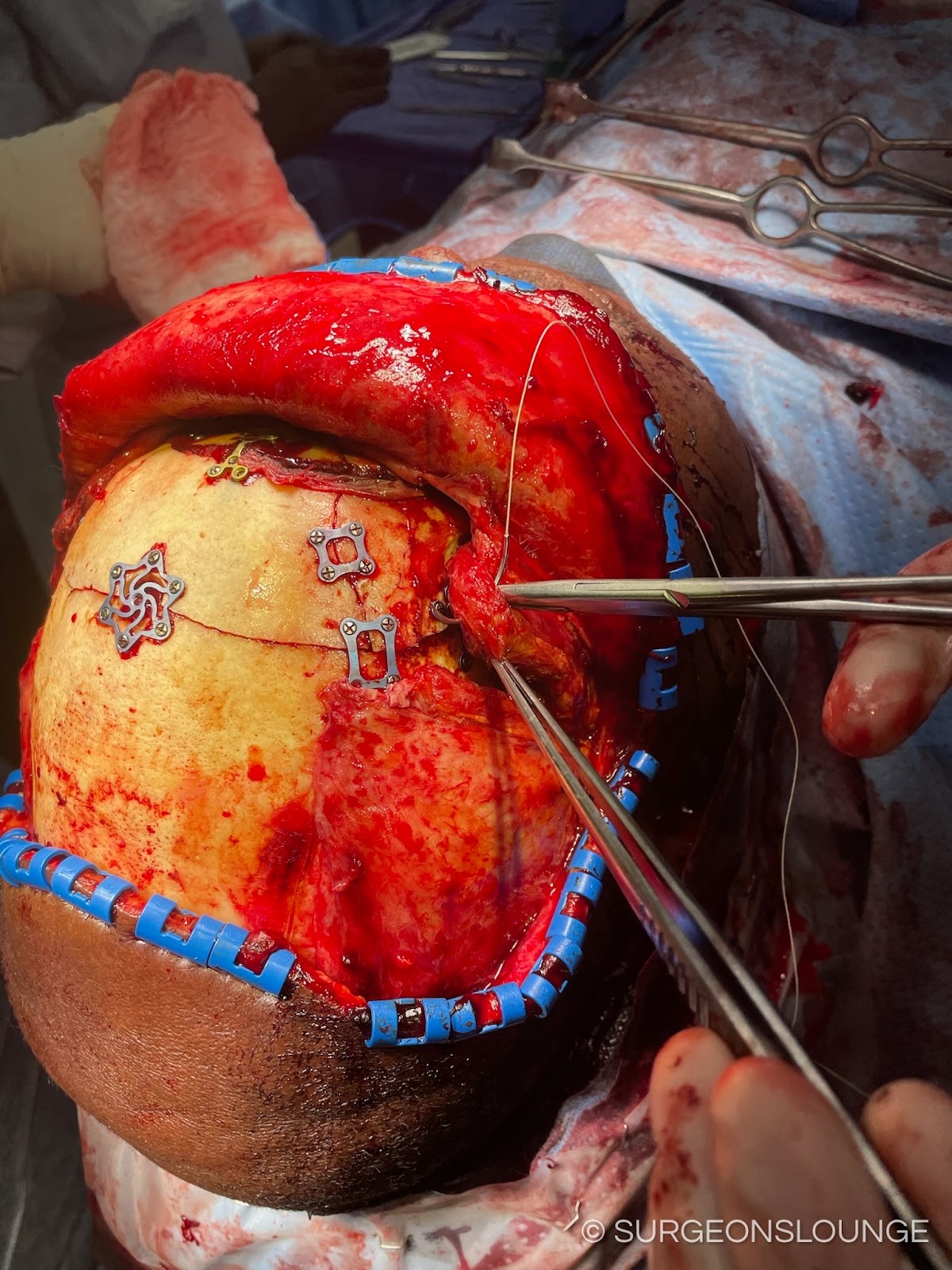
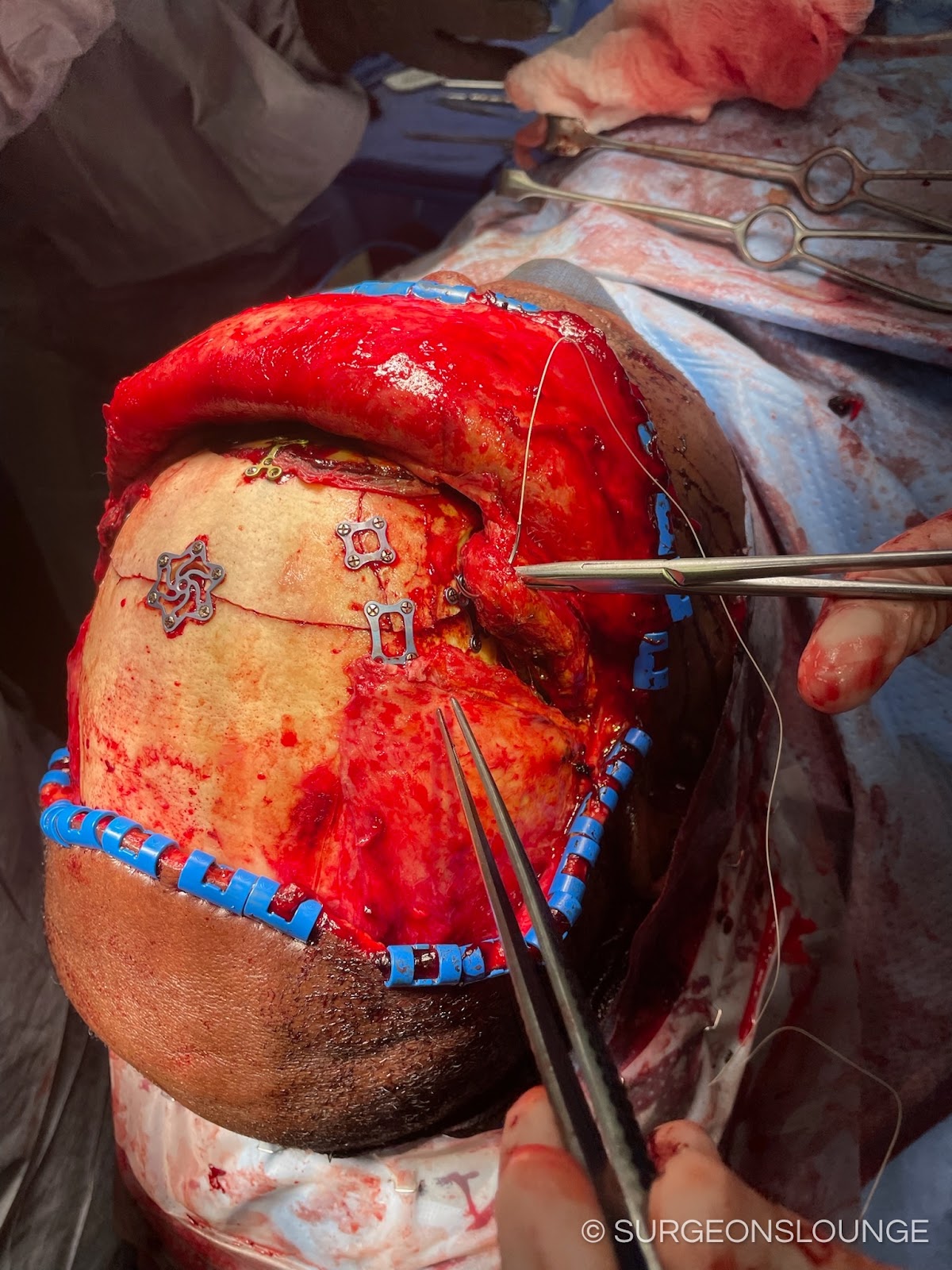
A #10 blade was used to create an incision at the proposed marking site to the supraperiosteal plane. A Kelly and curved stat was used to undermine the tissue posteriorly to allow placement of the Raney clips. Raney clips were placed at the anterior and posterior portions of the incision.
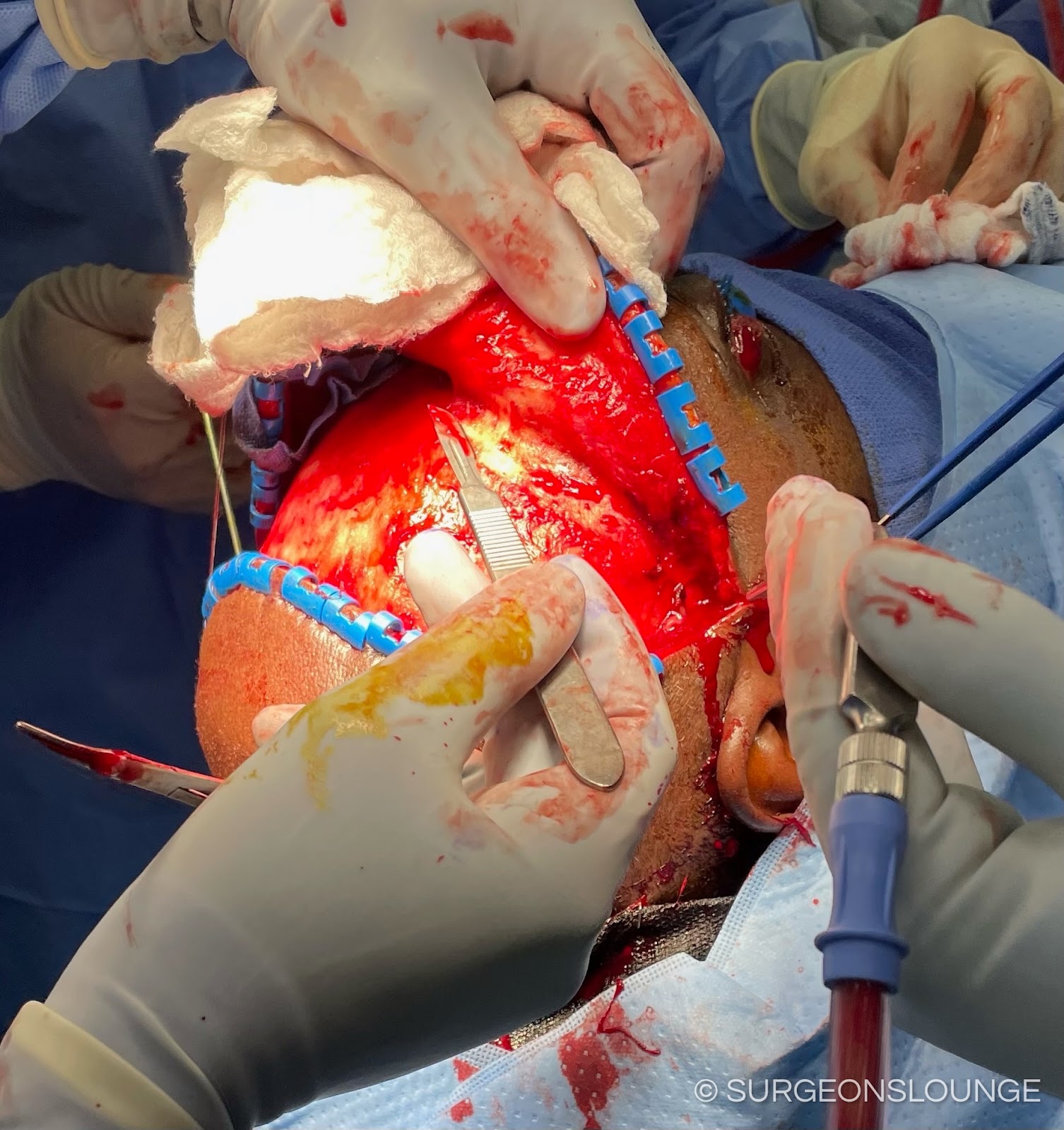
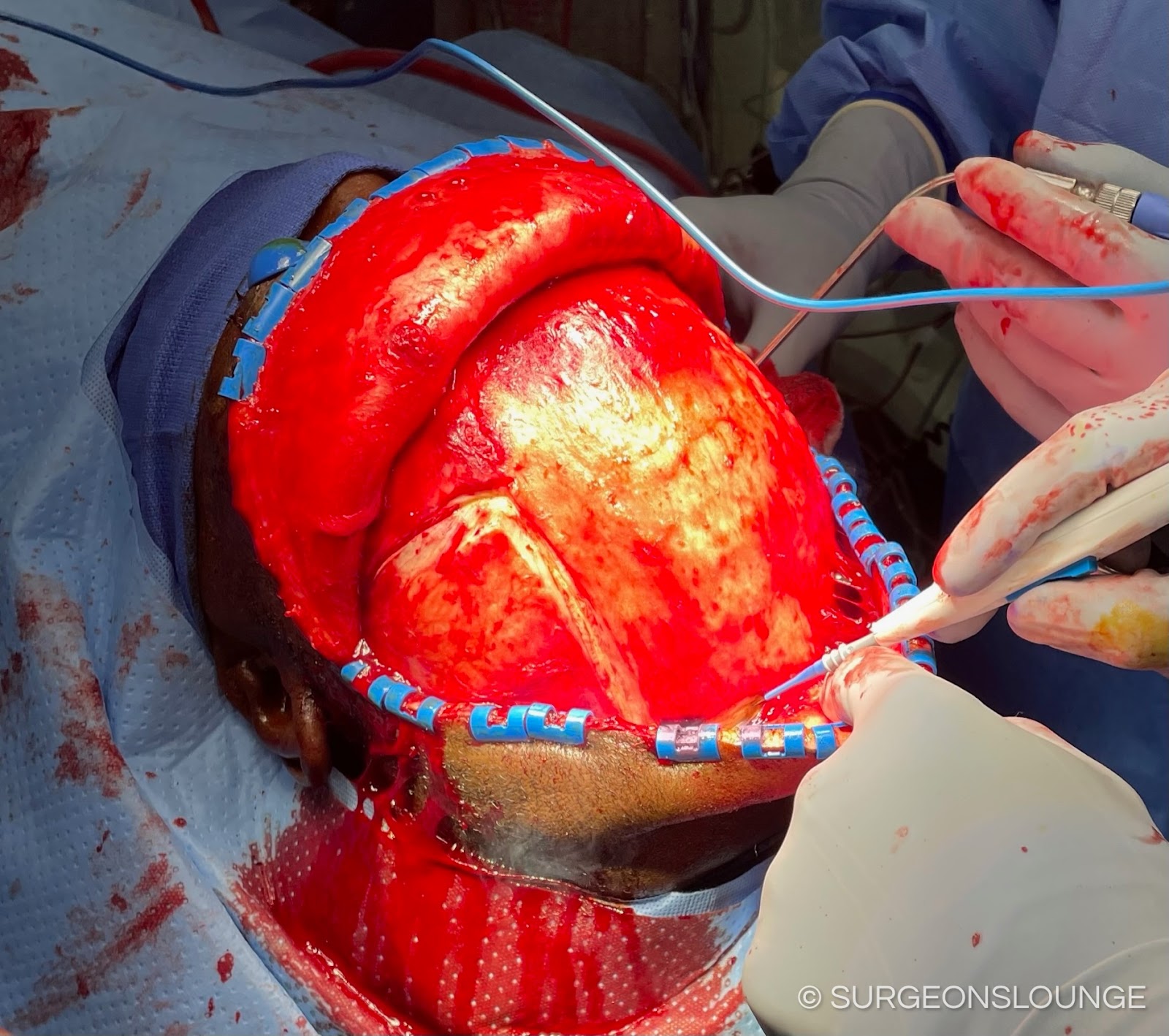
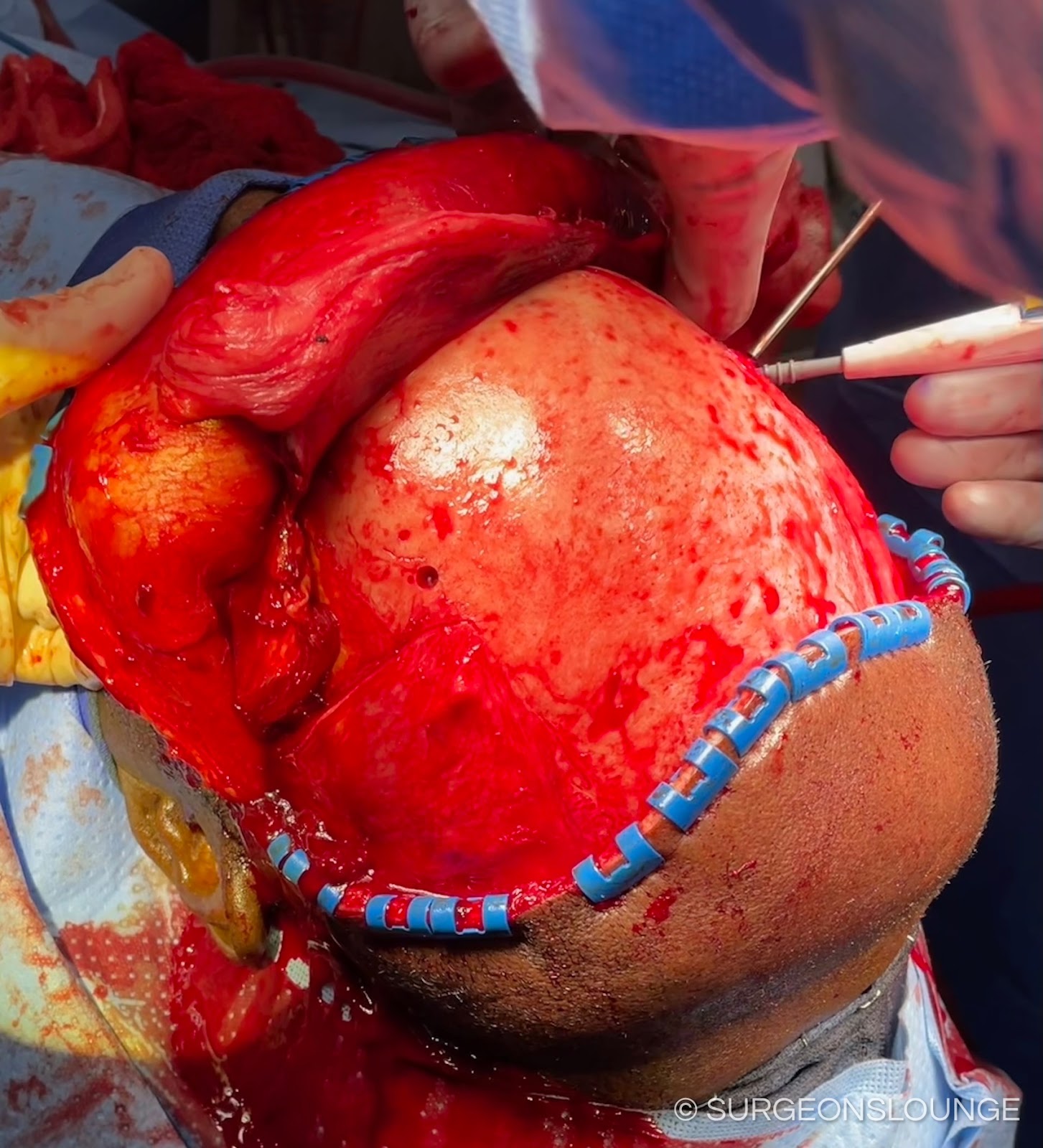
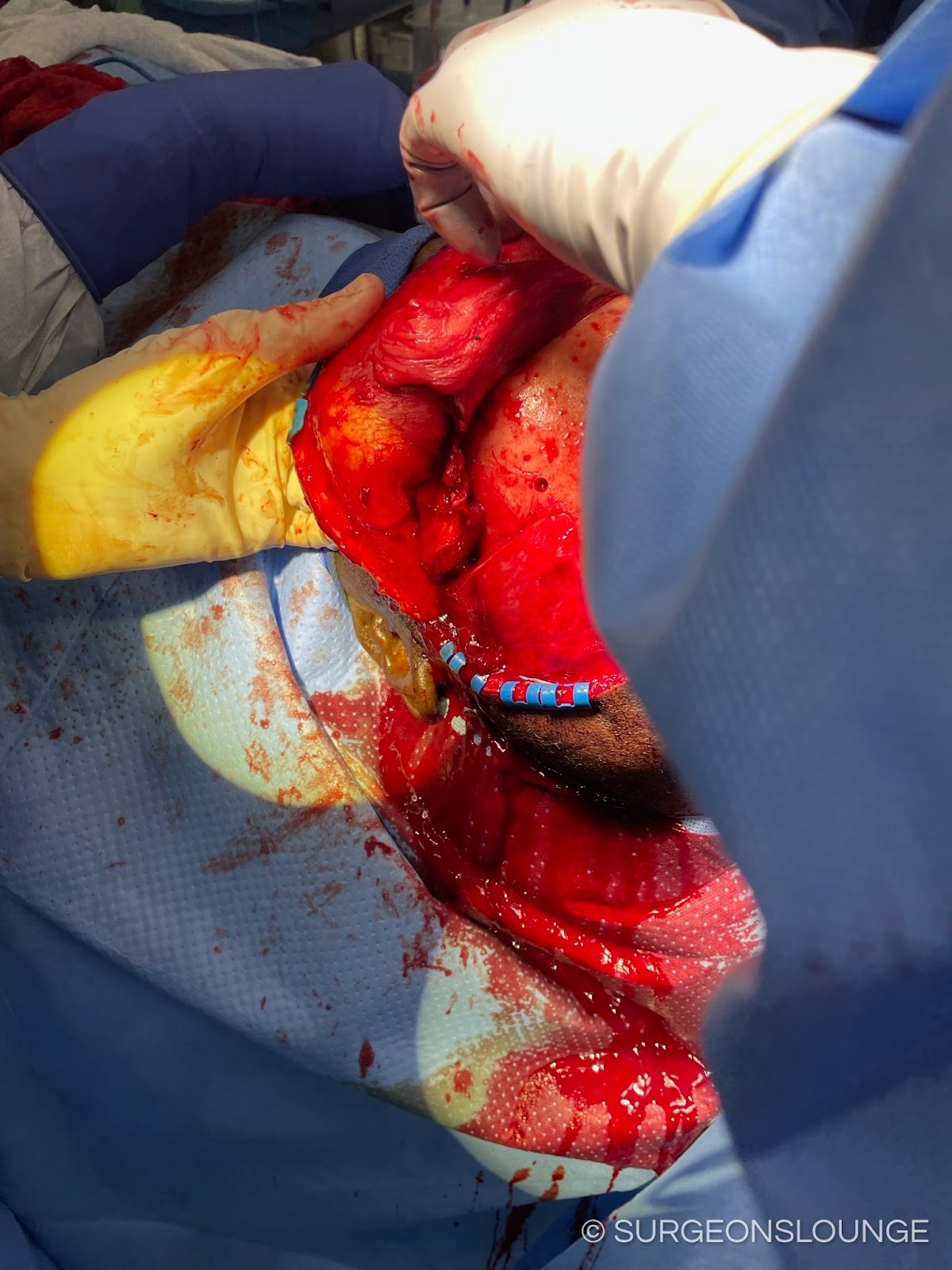
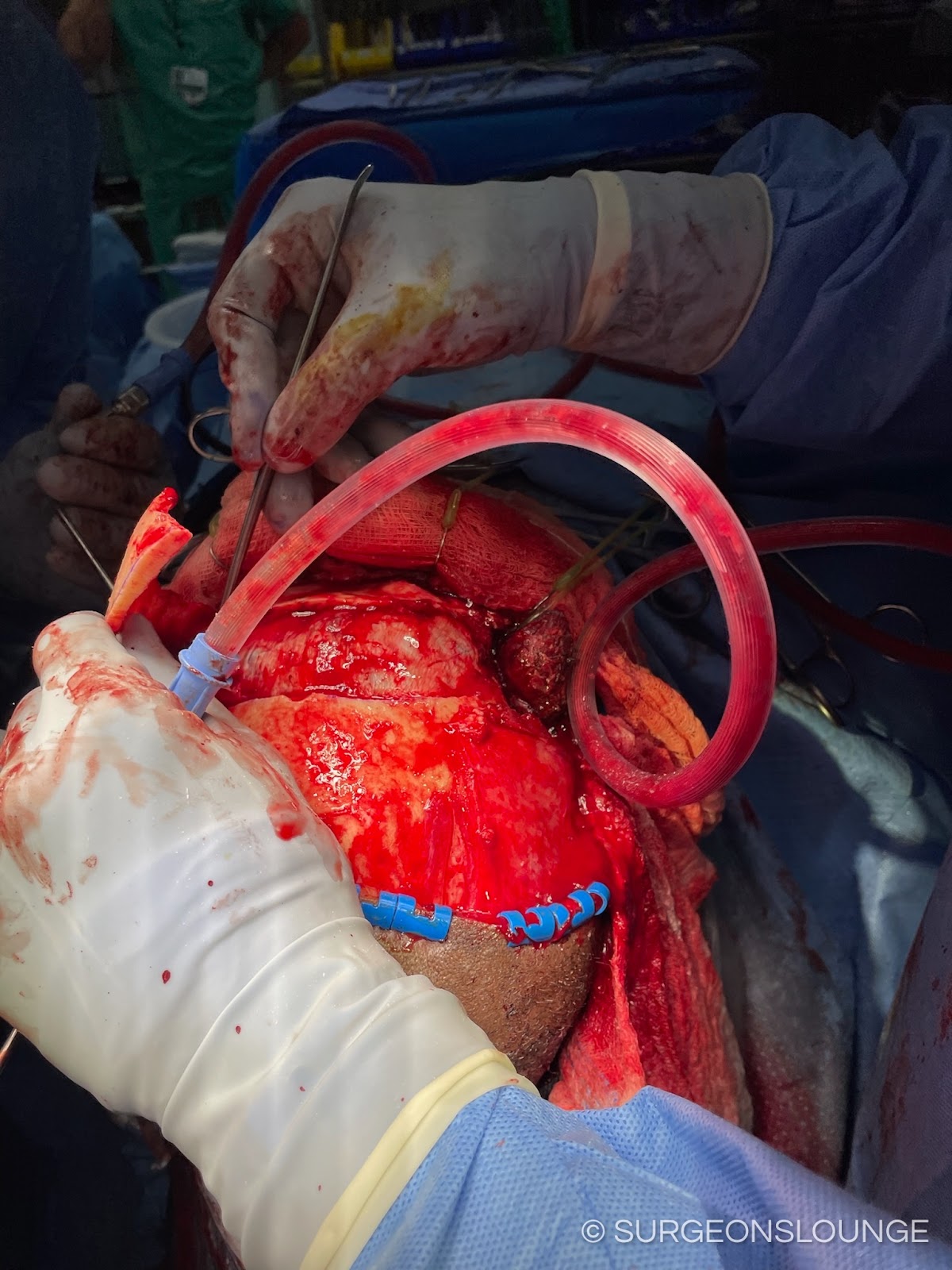
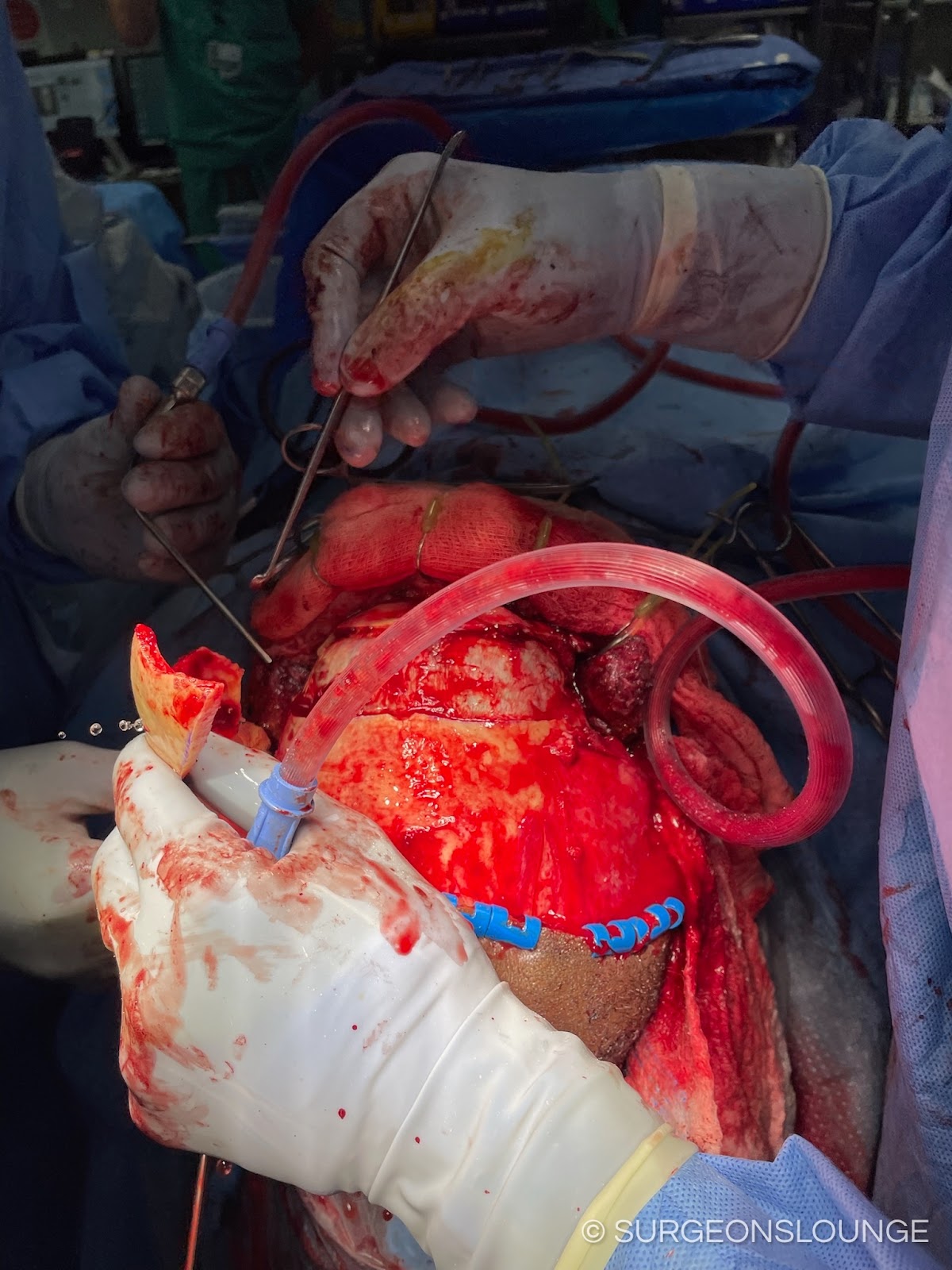
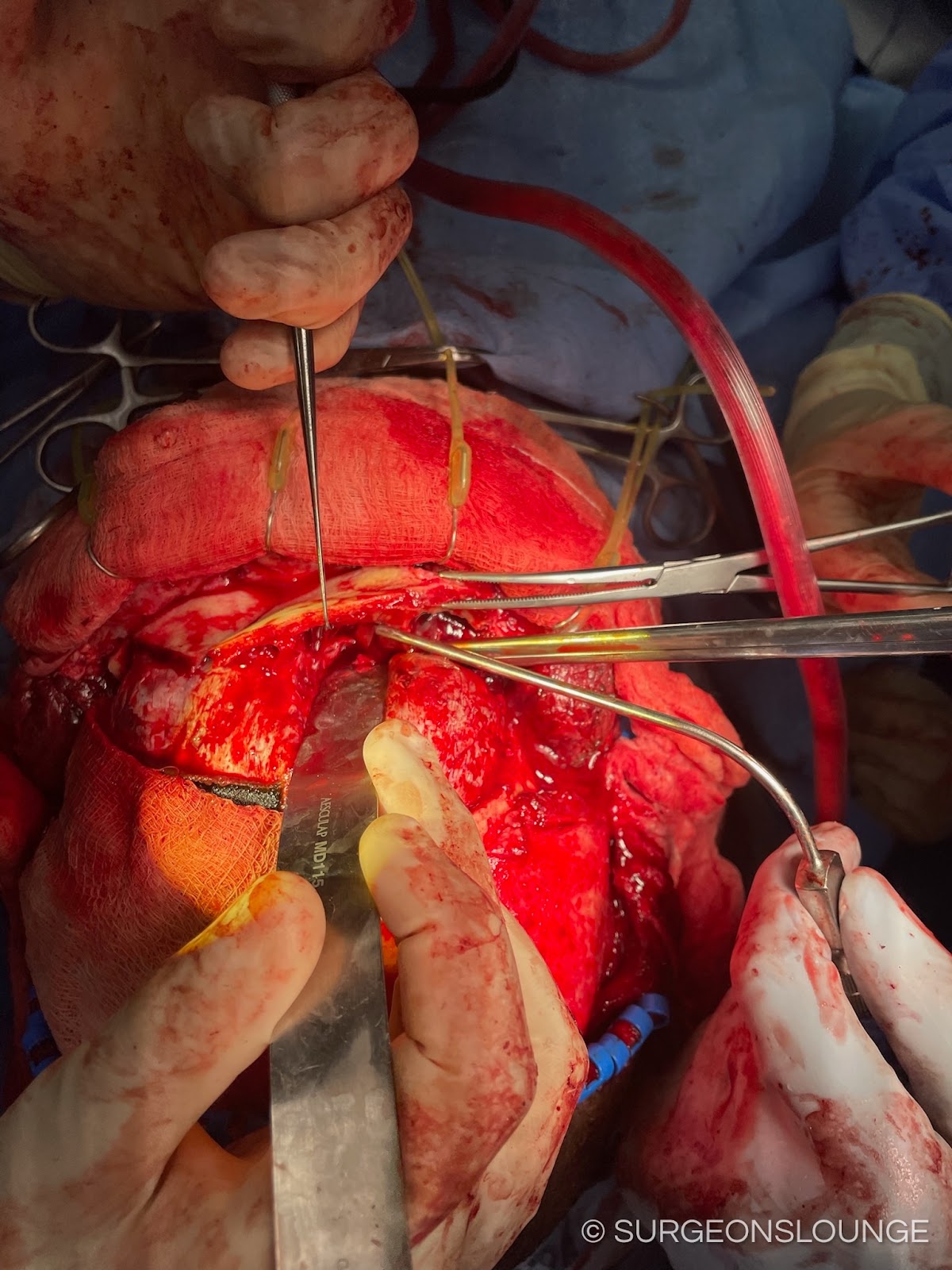
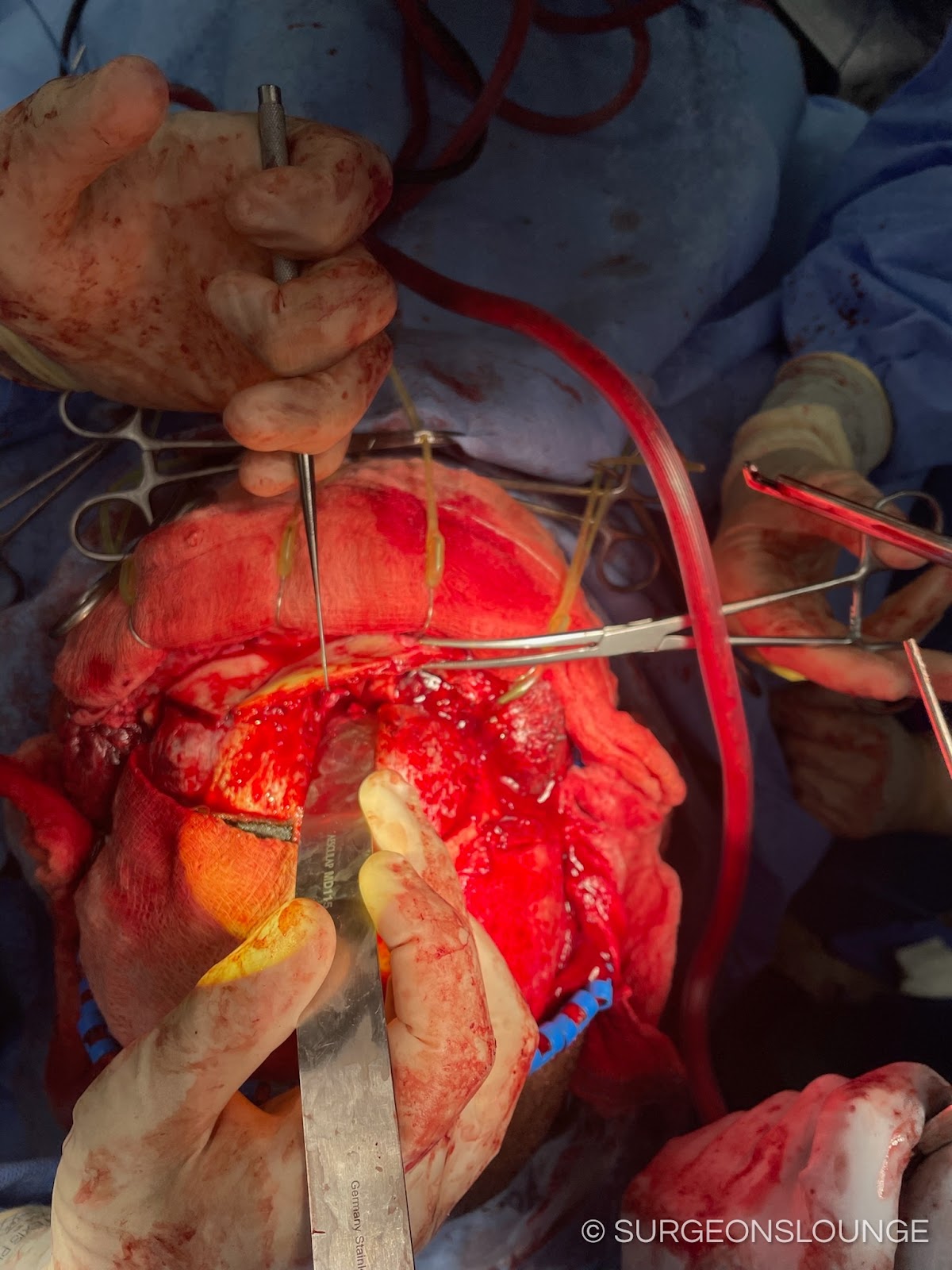
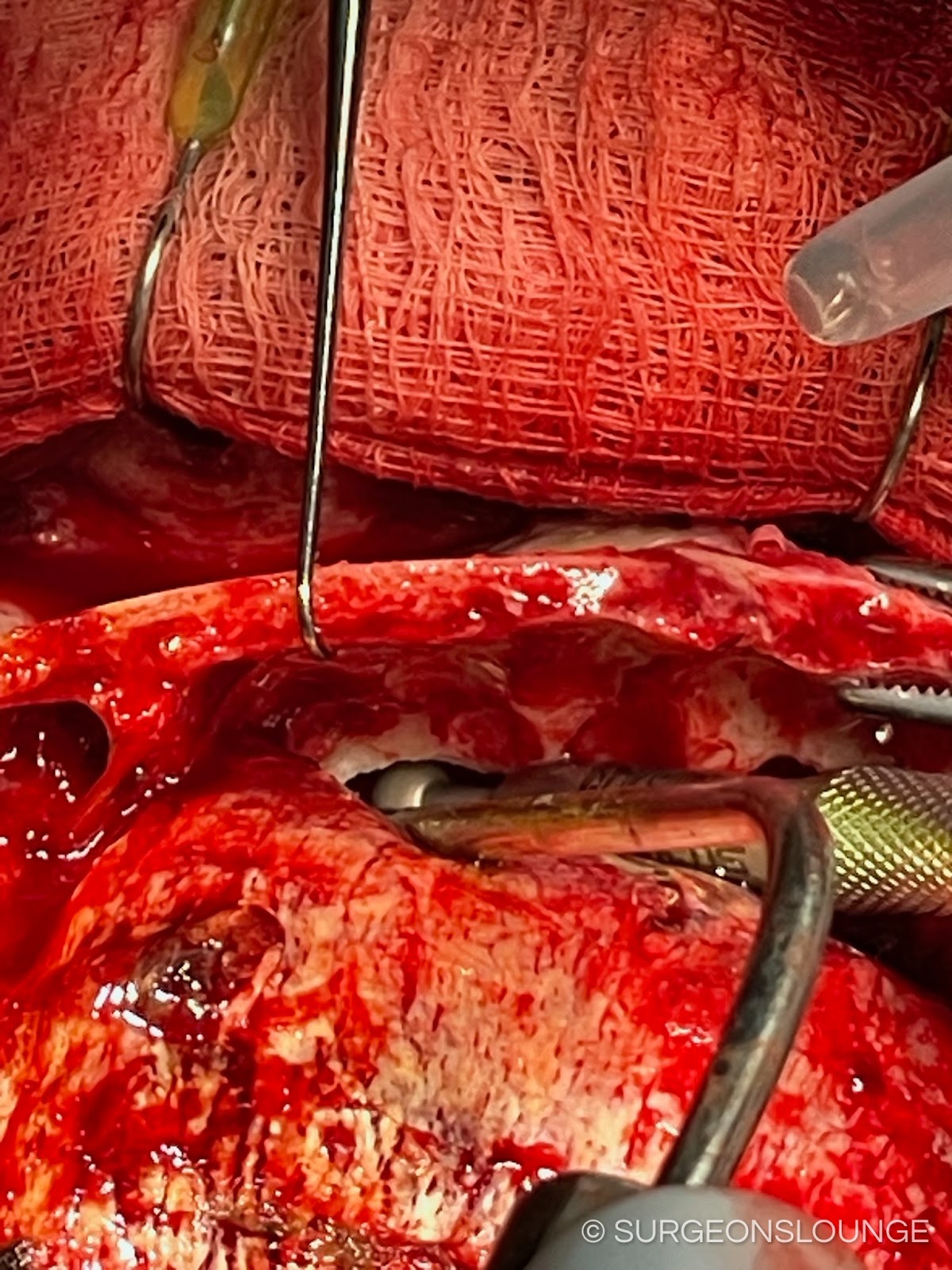
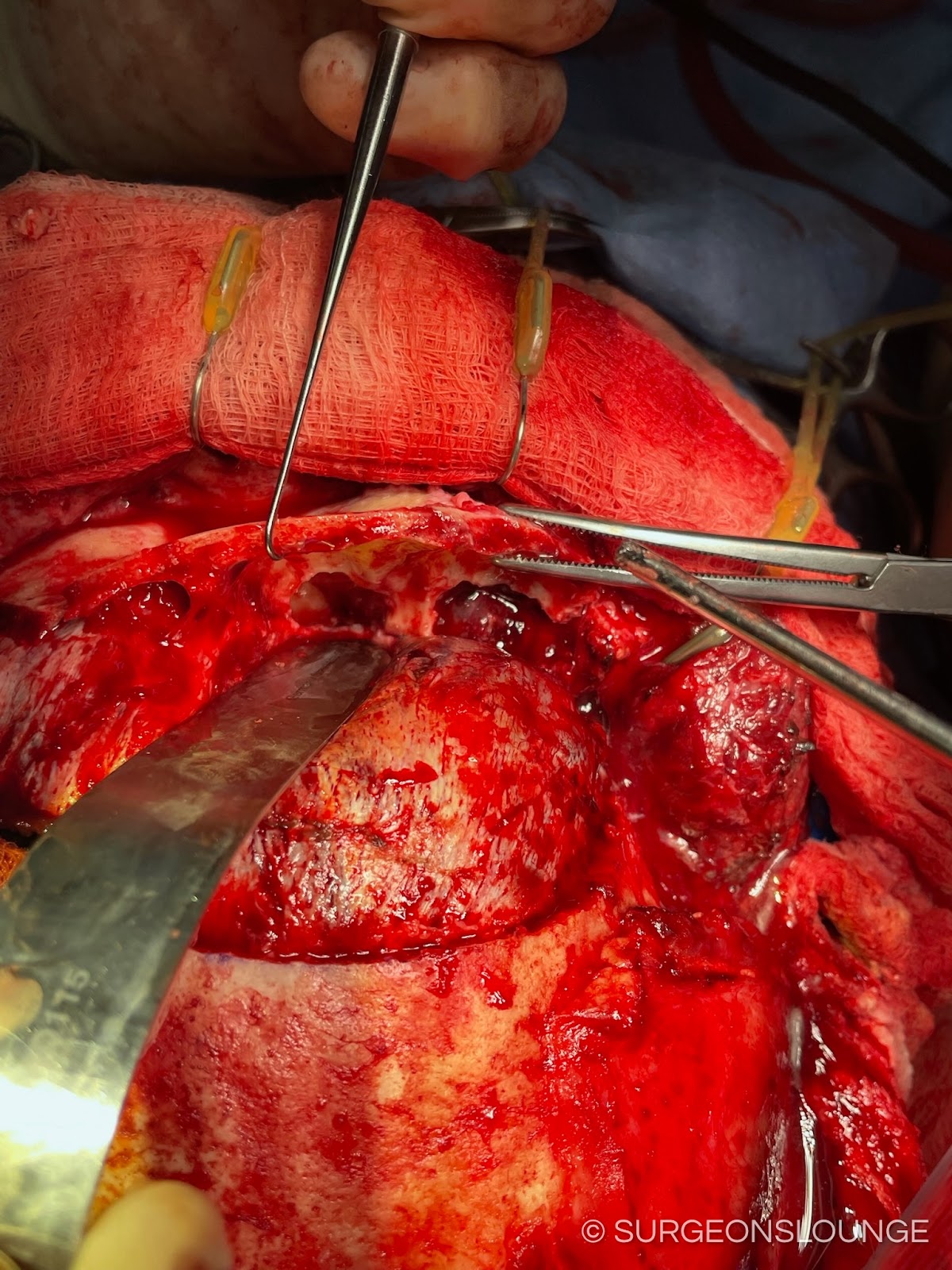
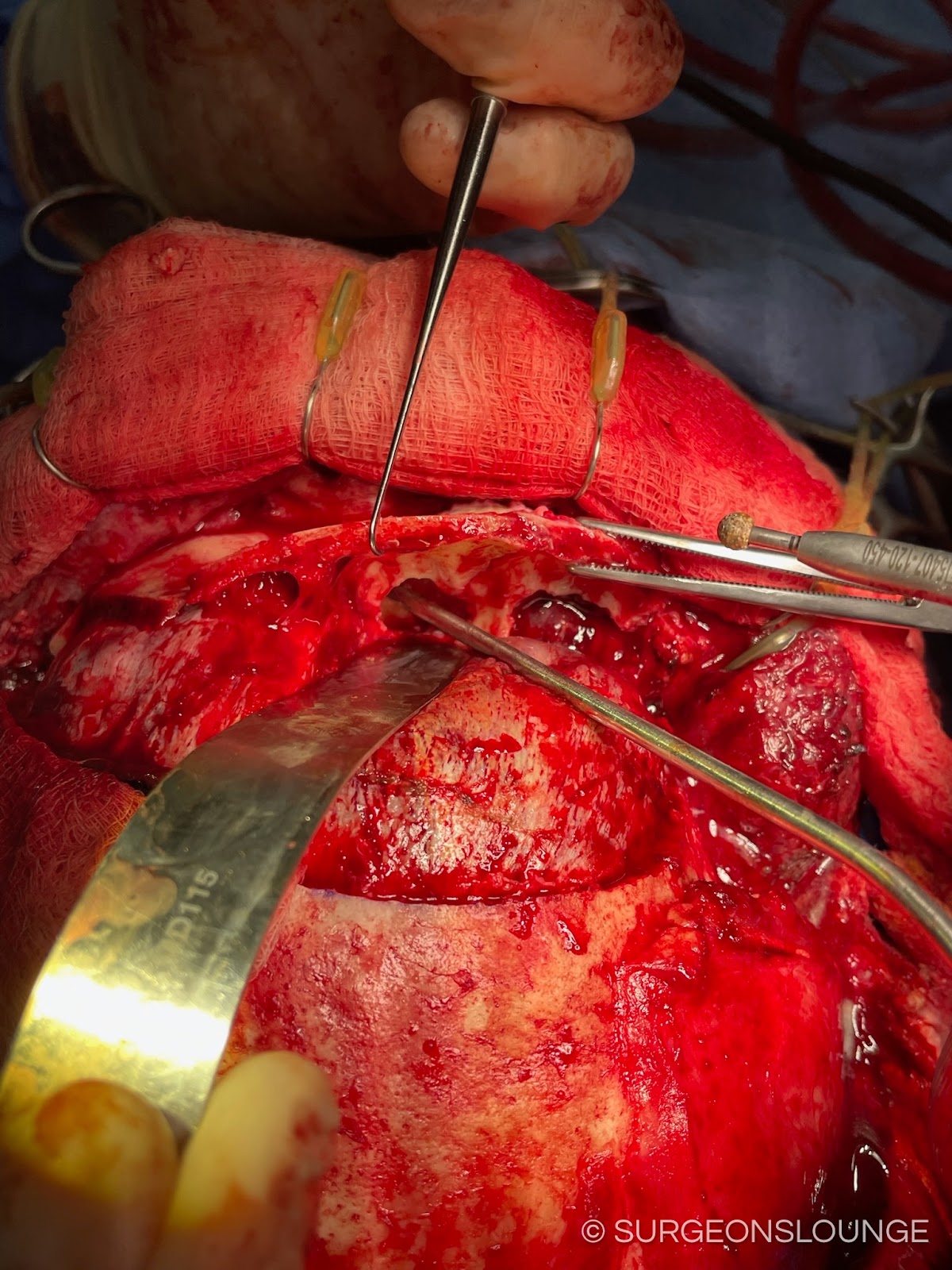
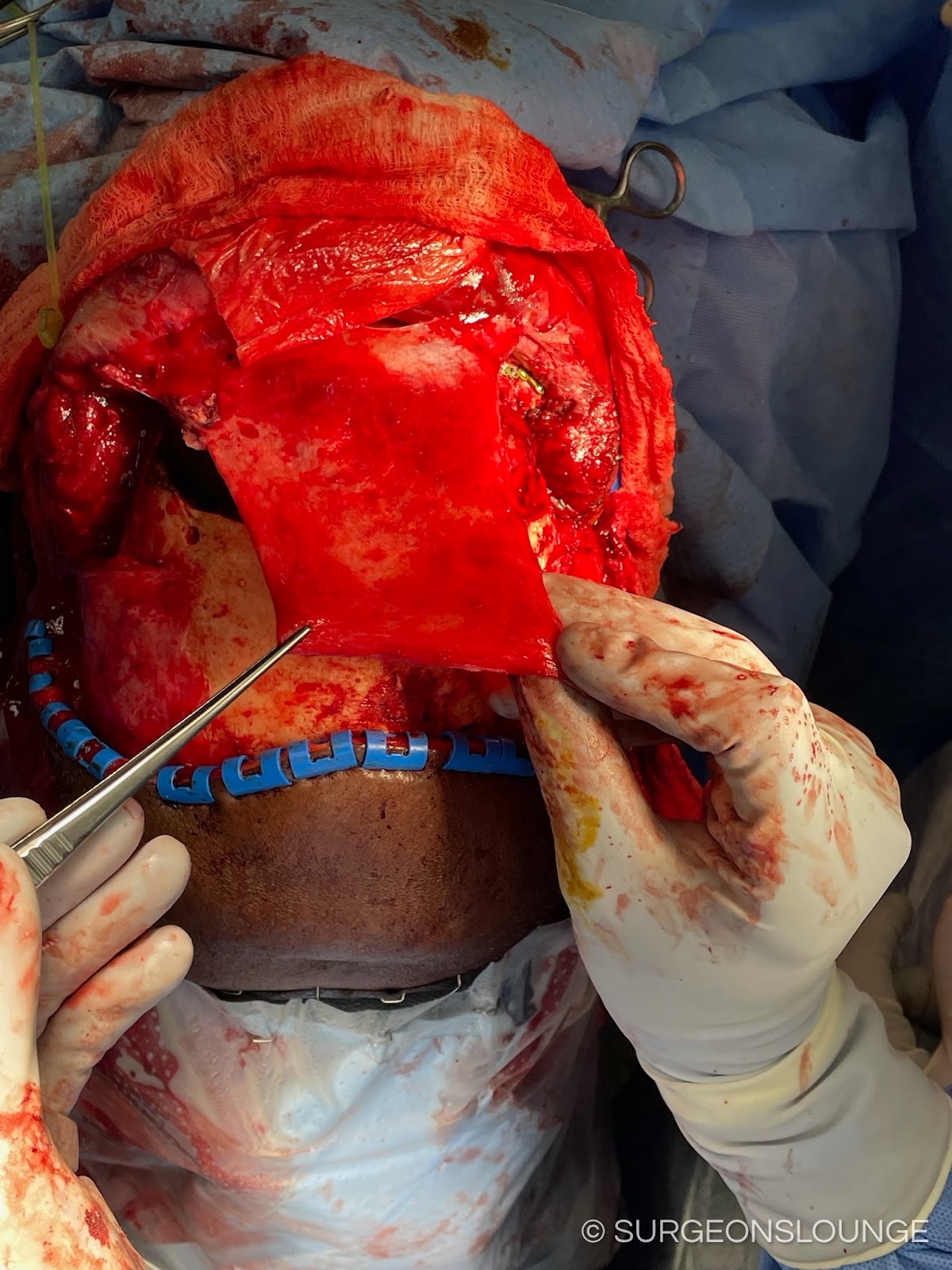
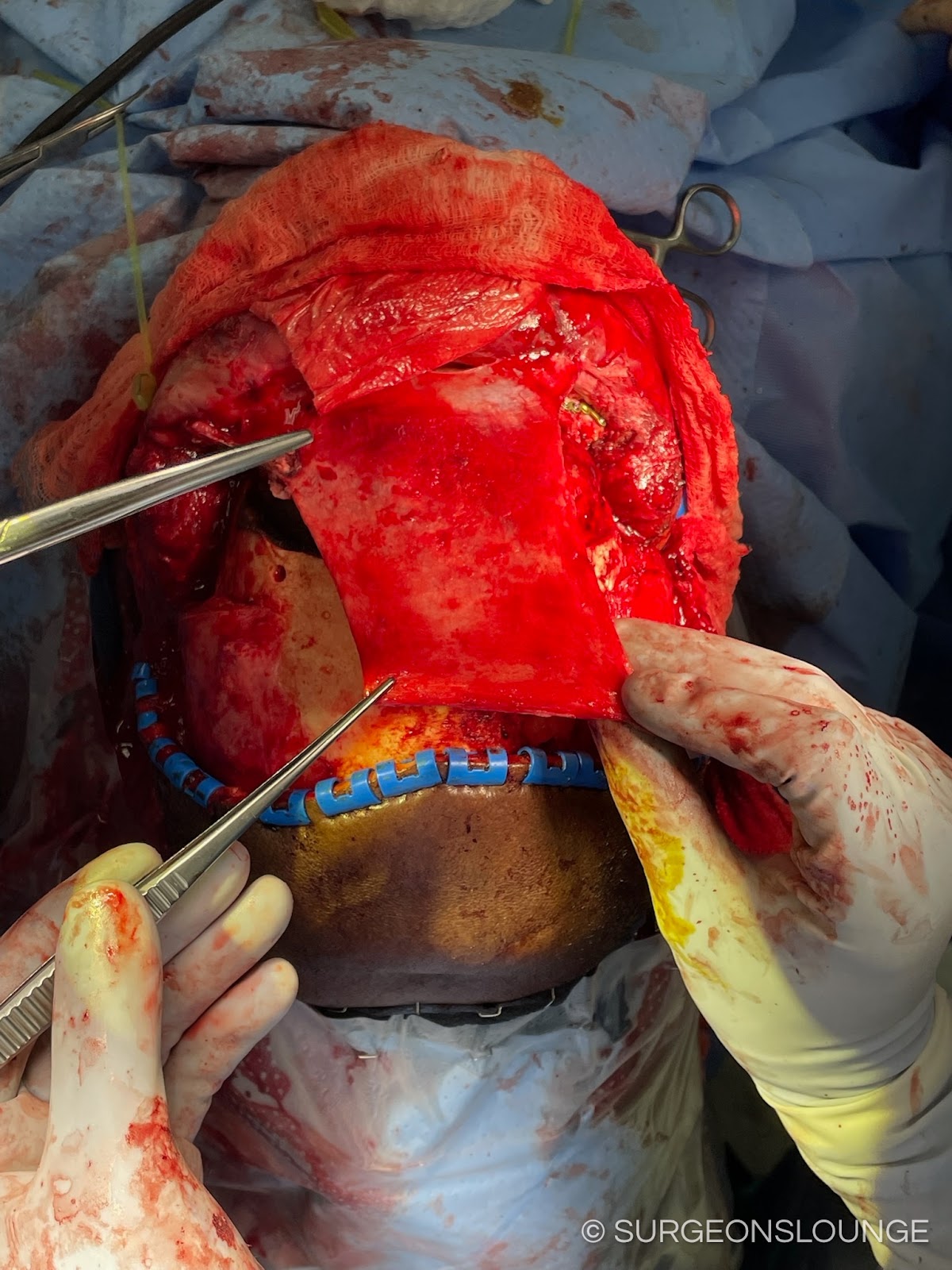
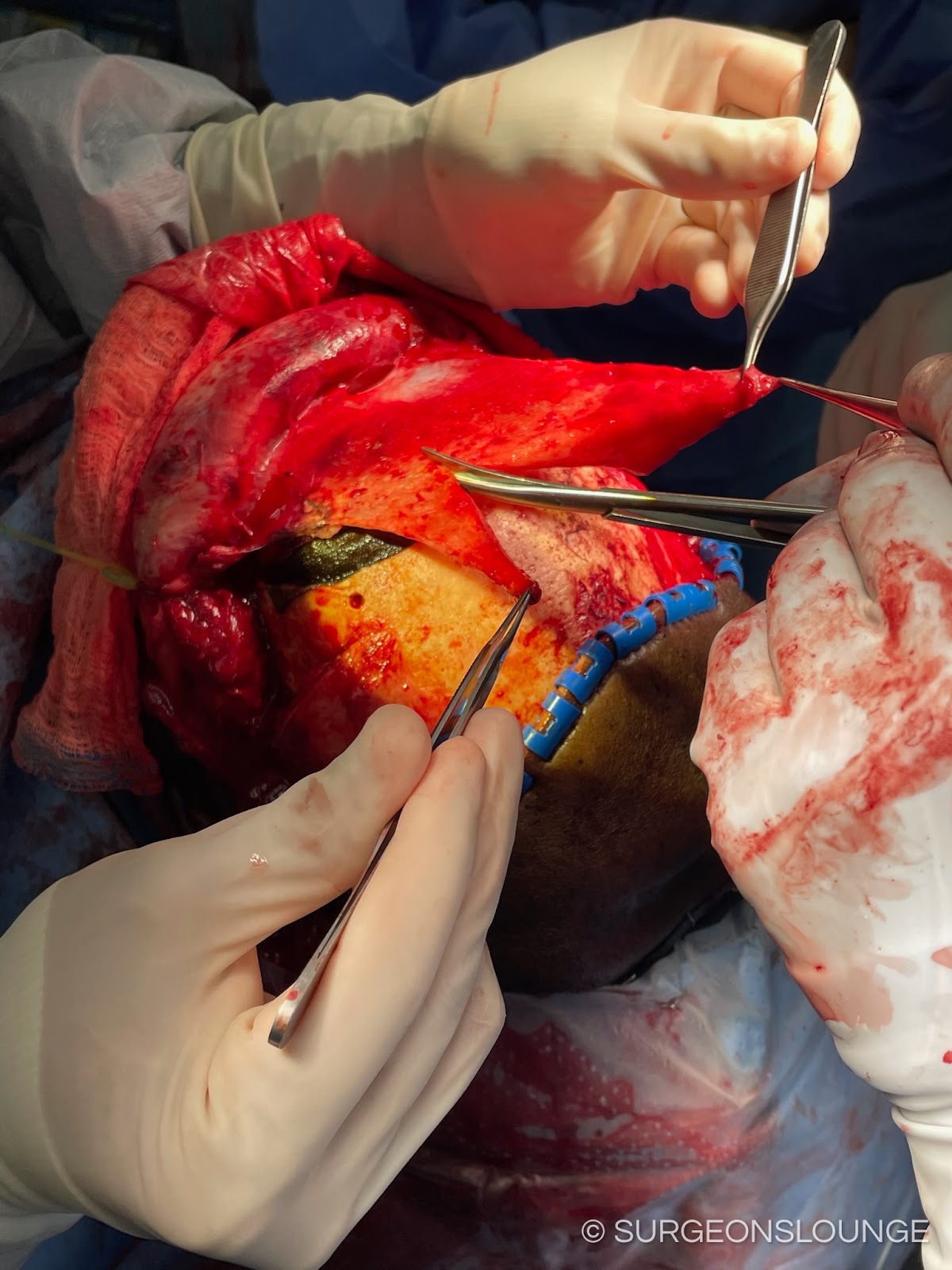
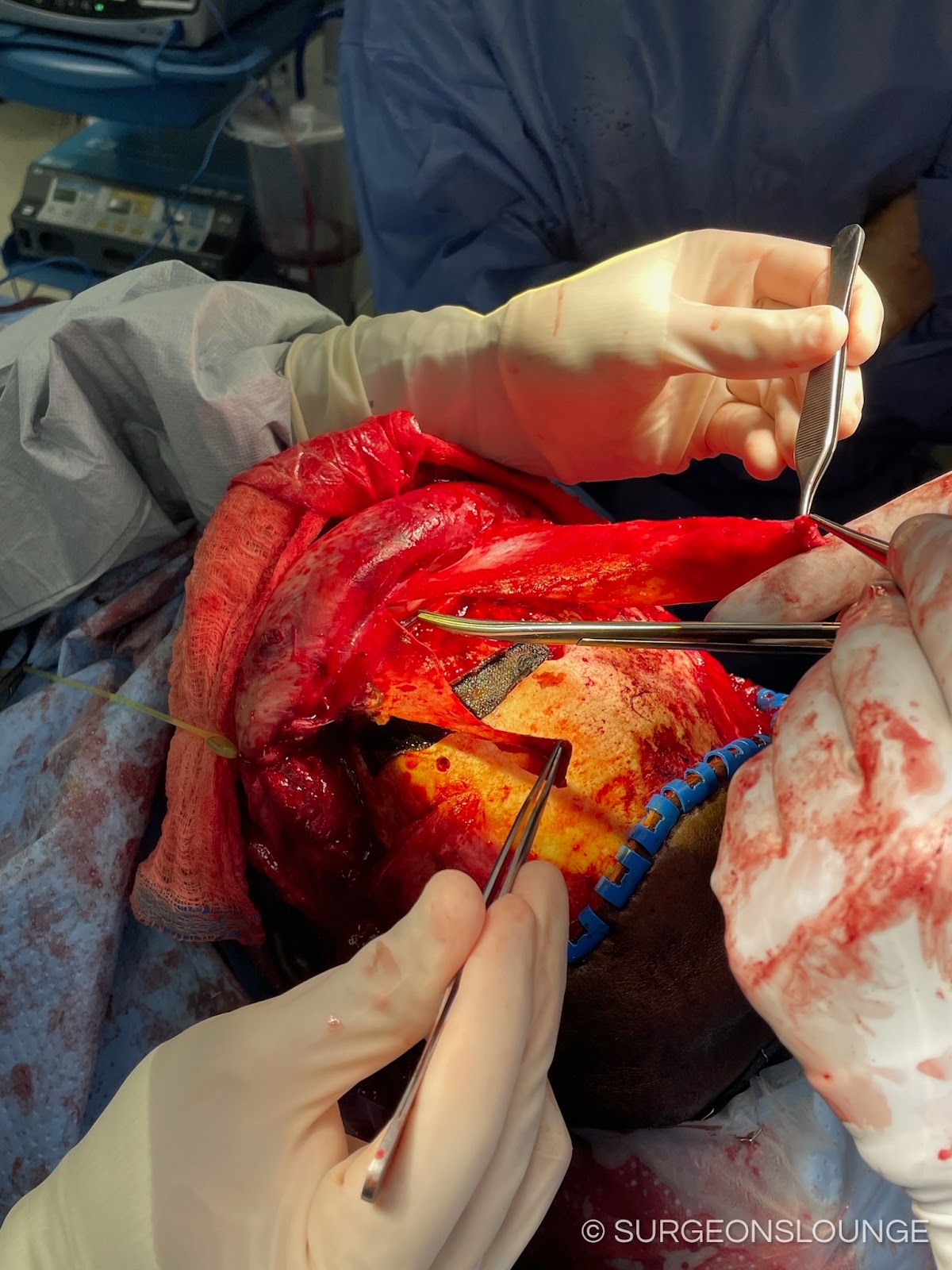
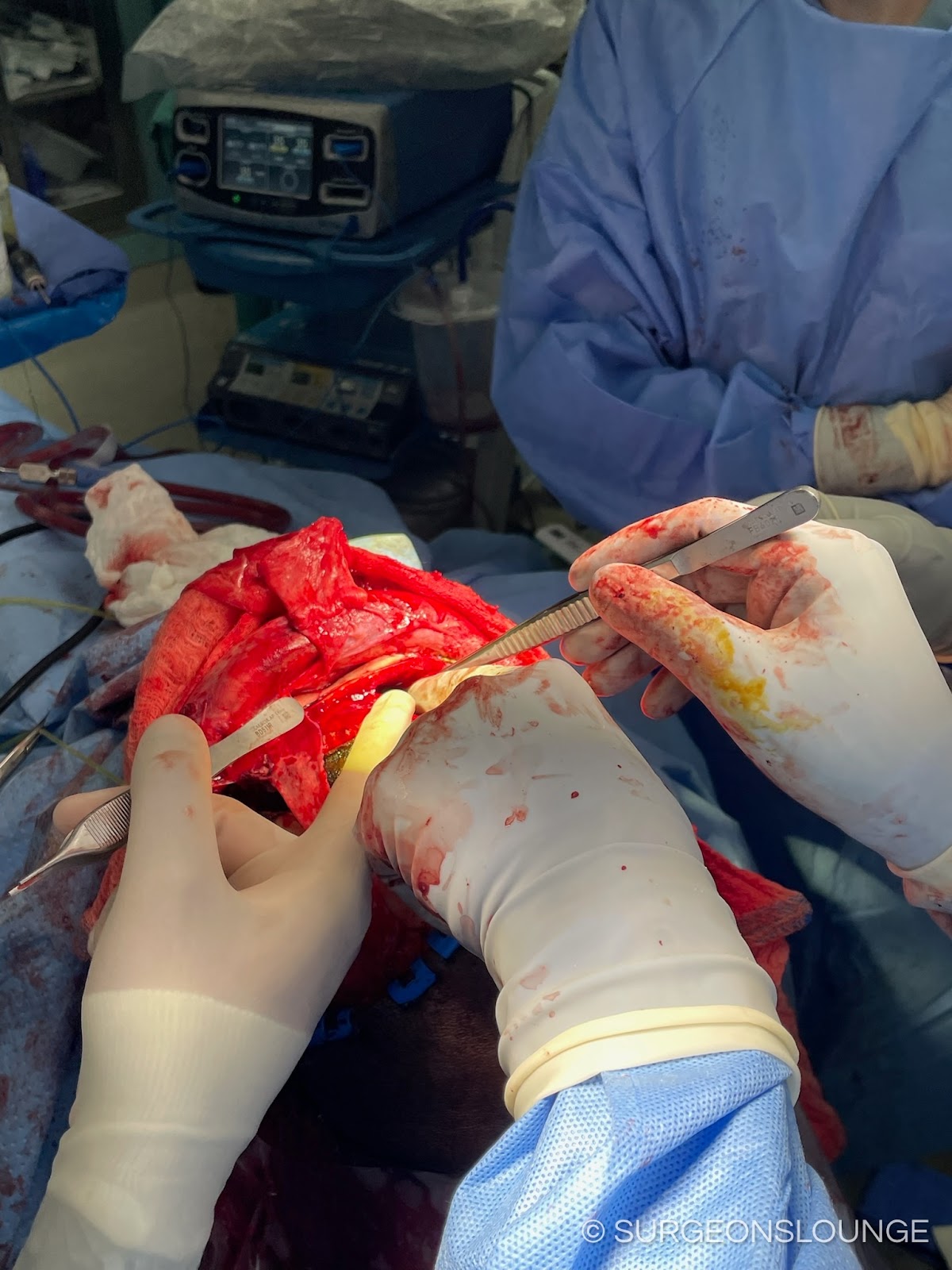
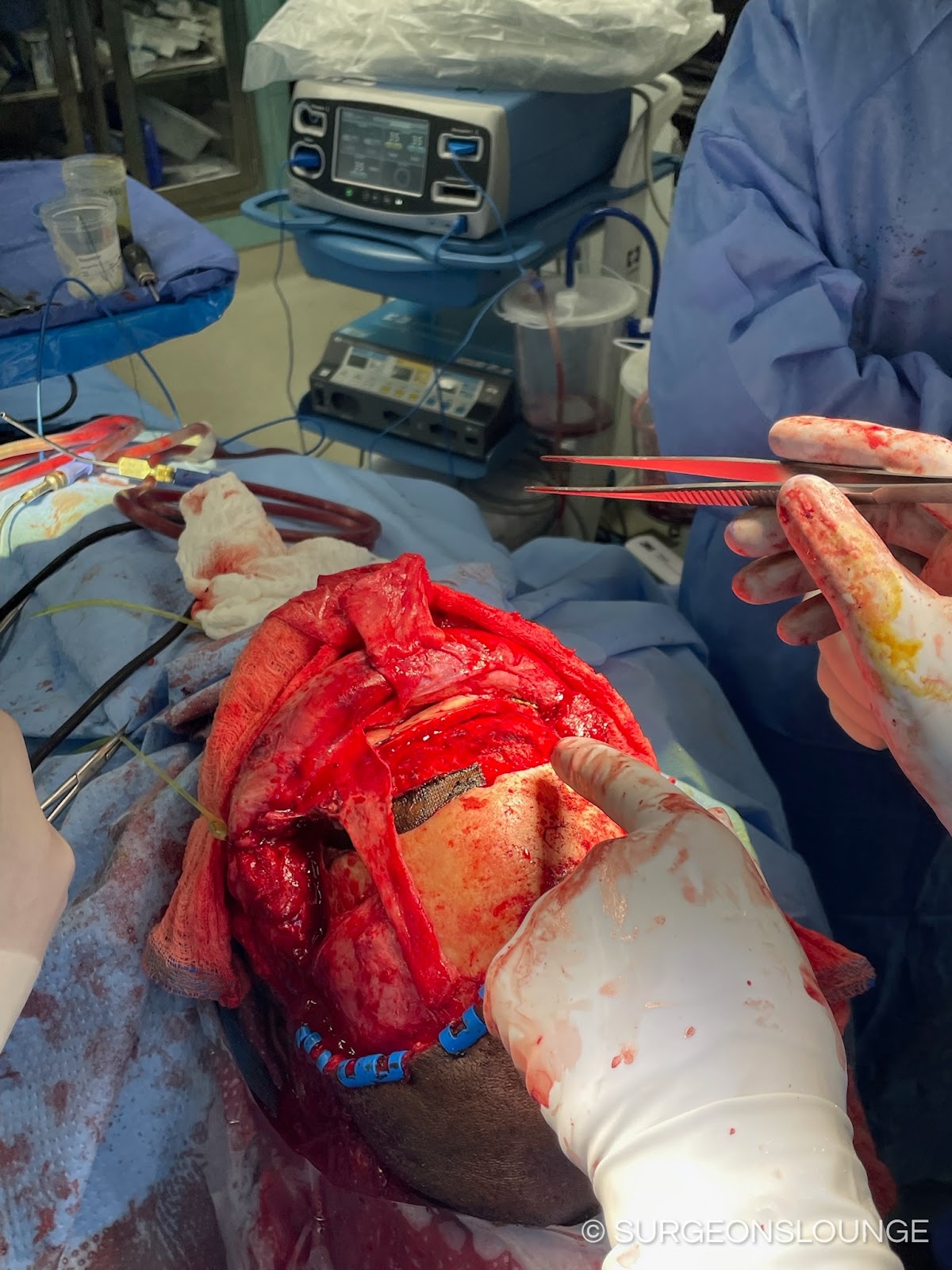
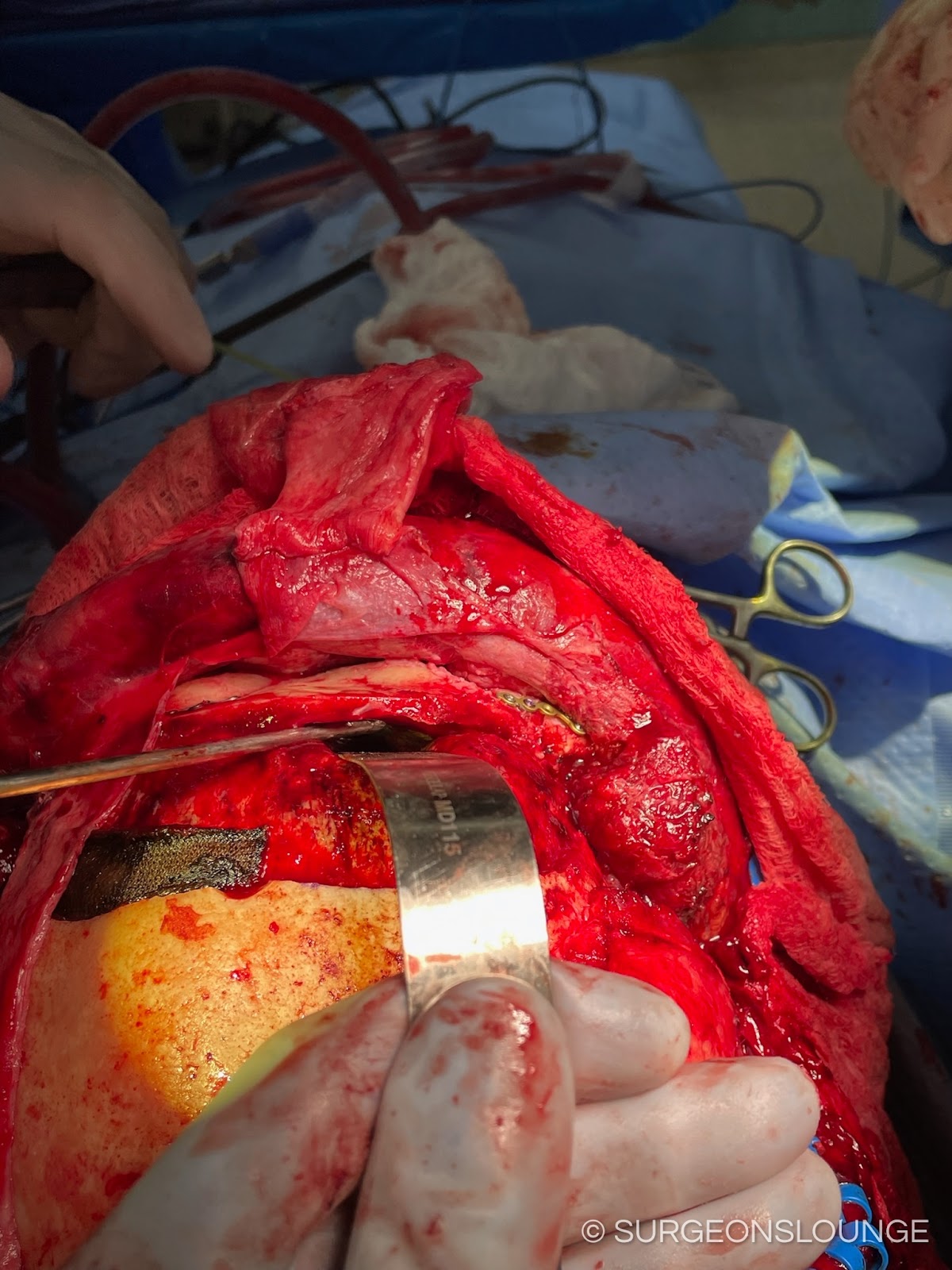
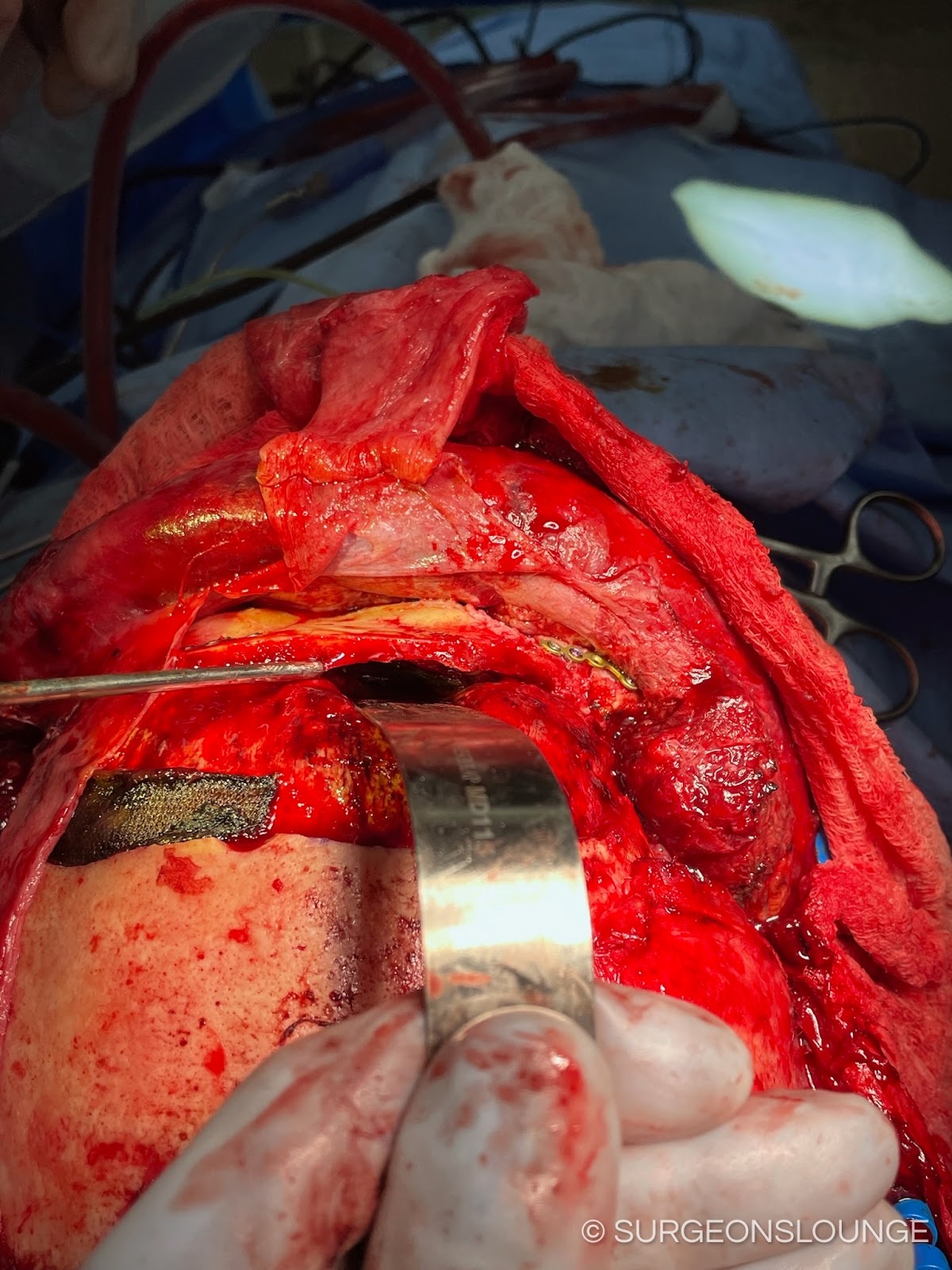
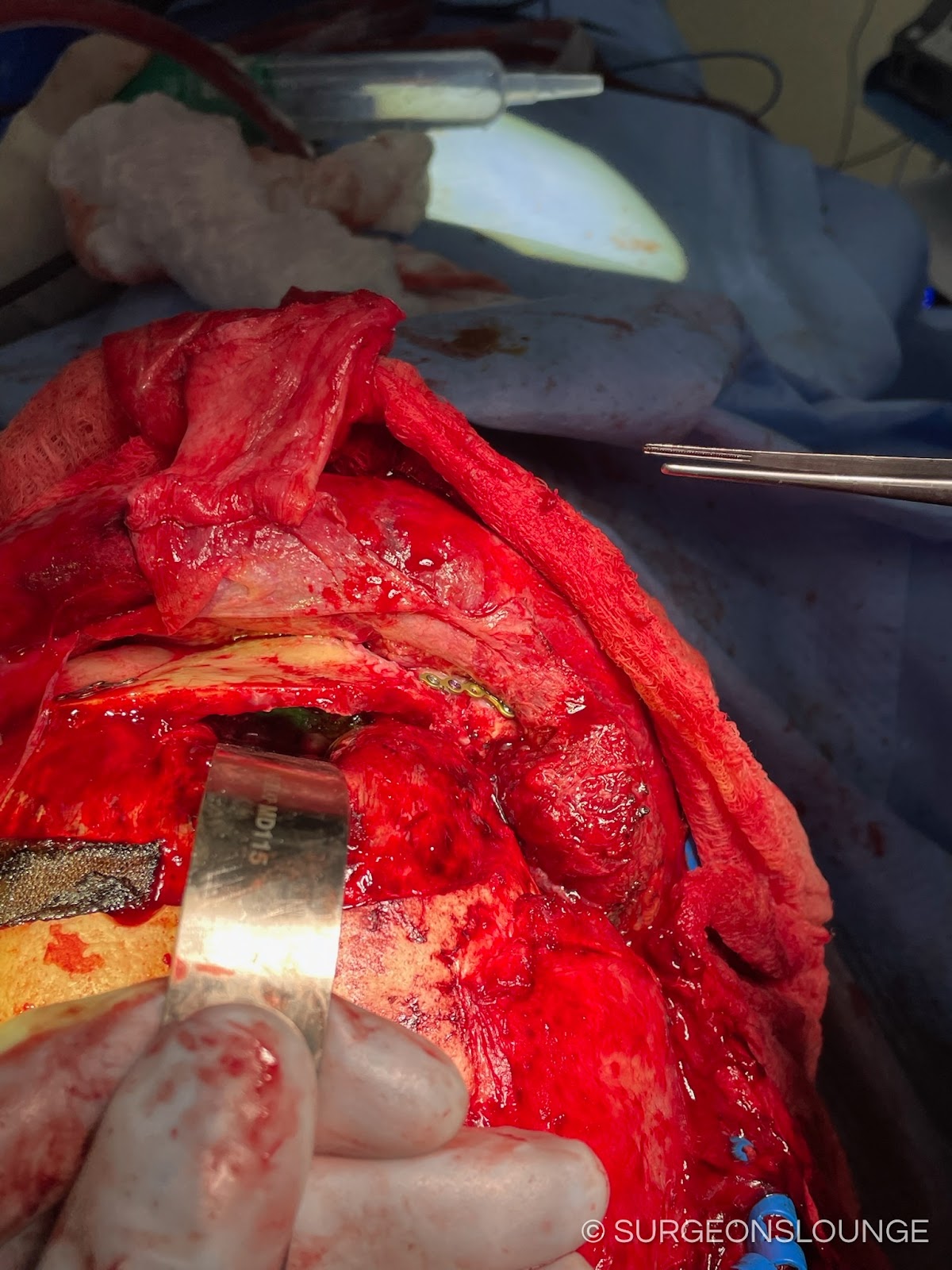
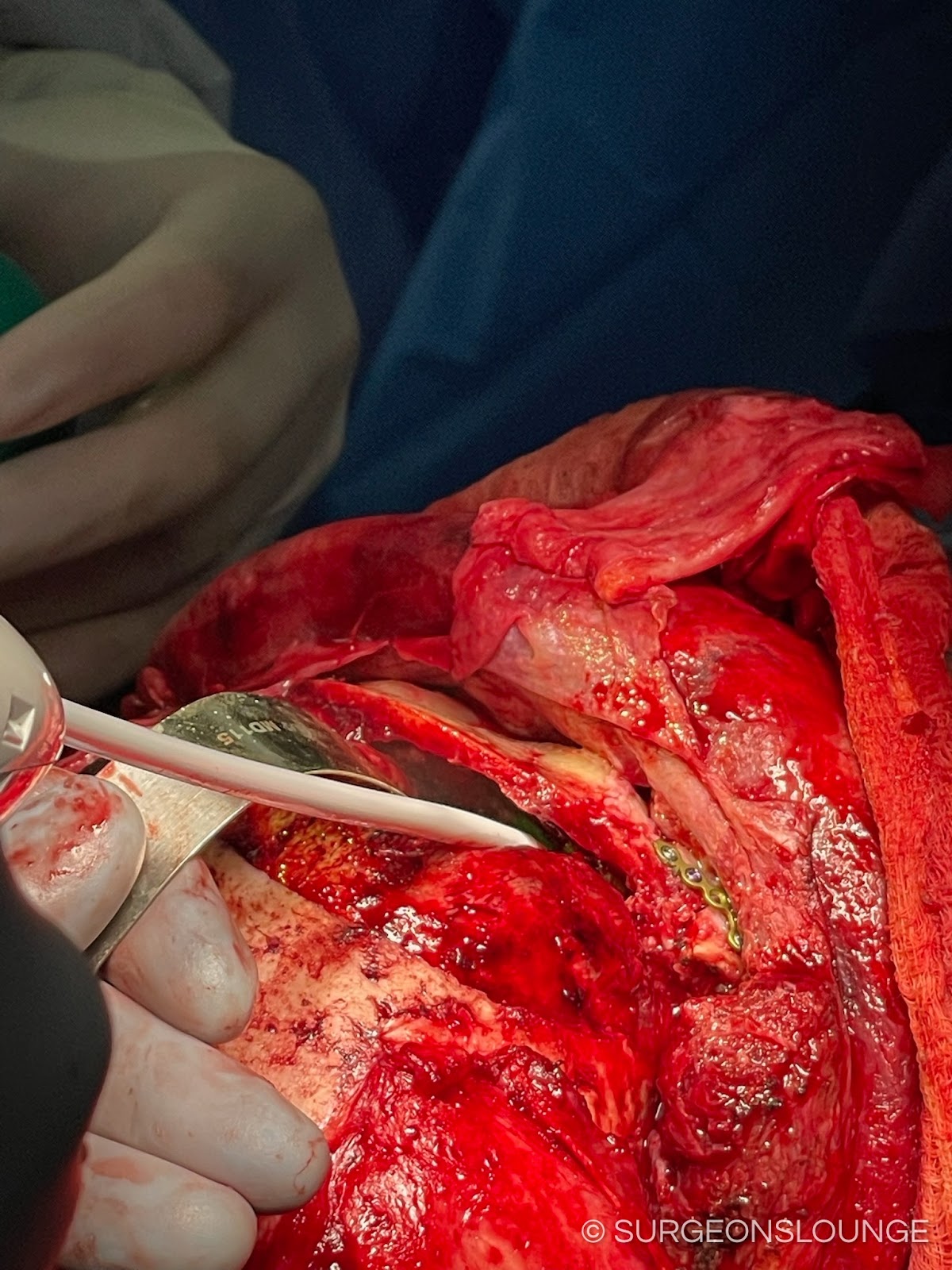
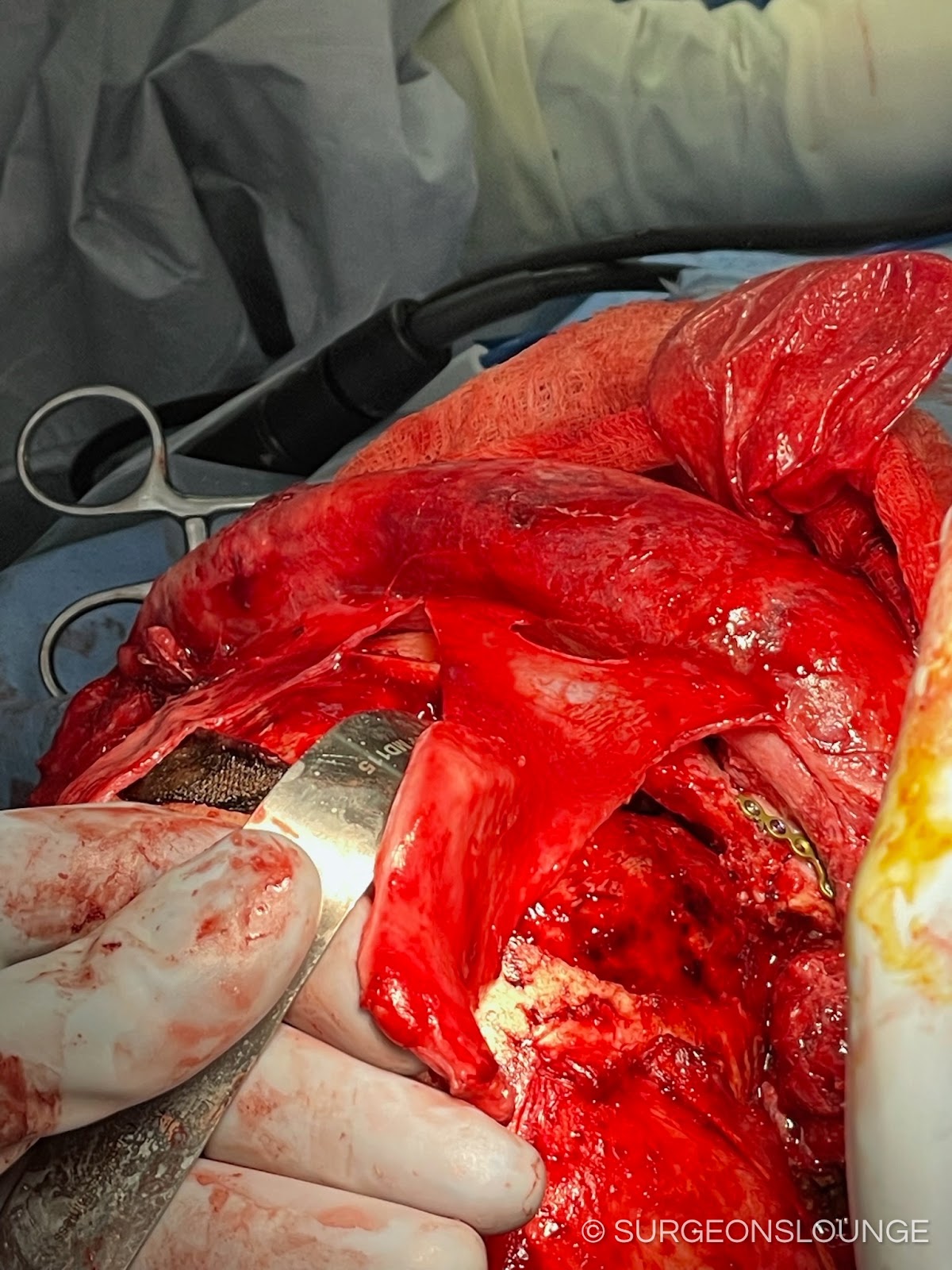
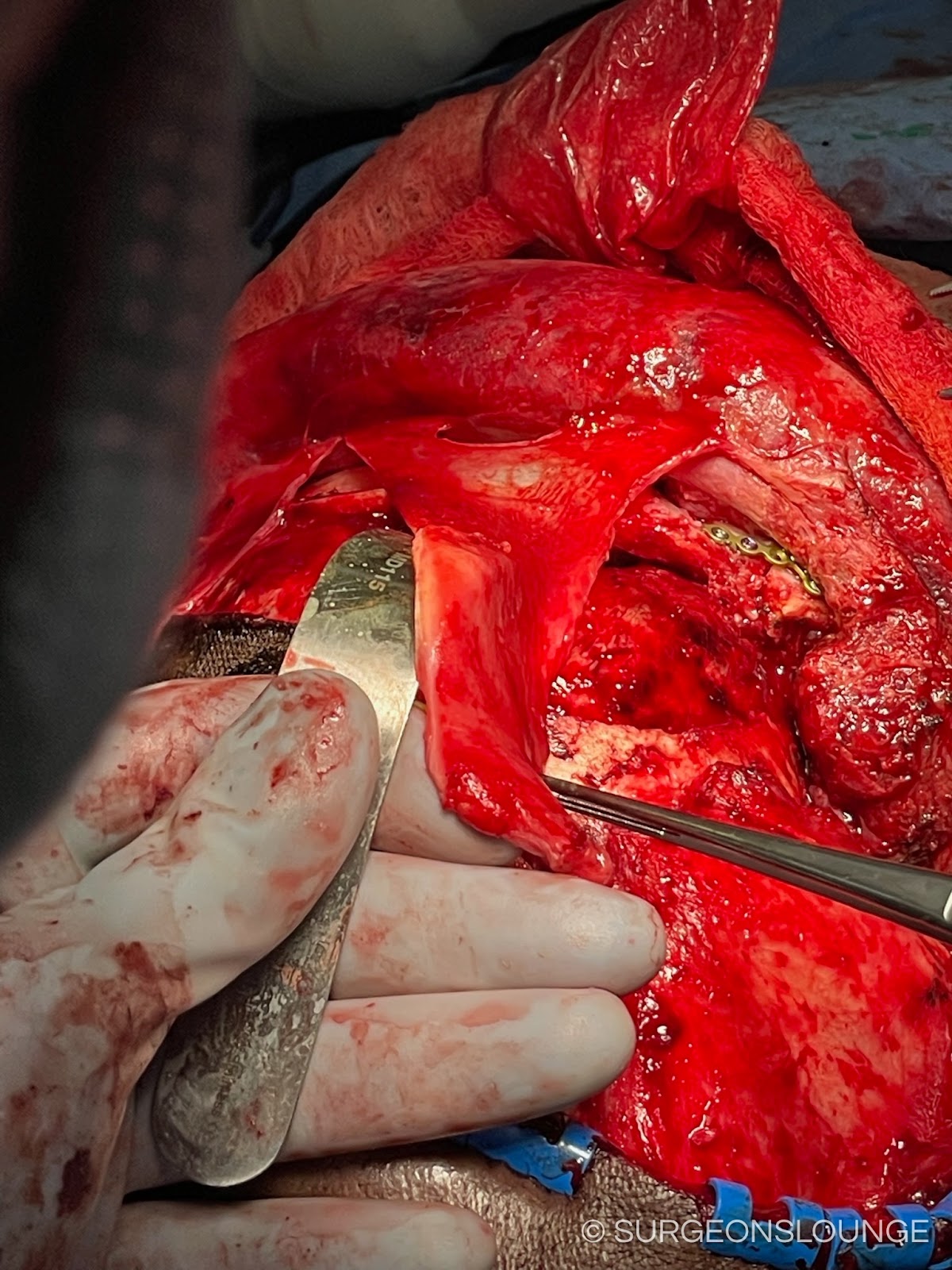
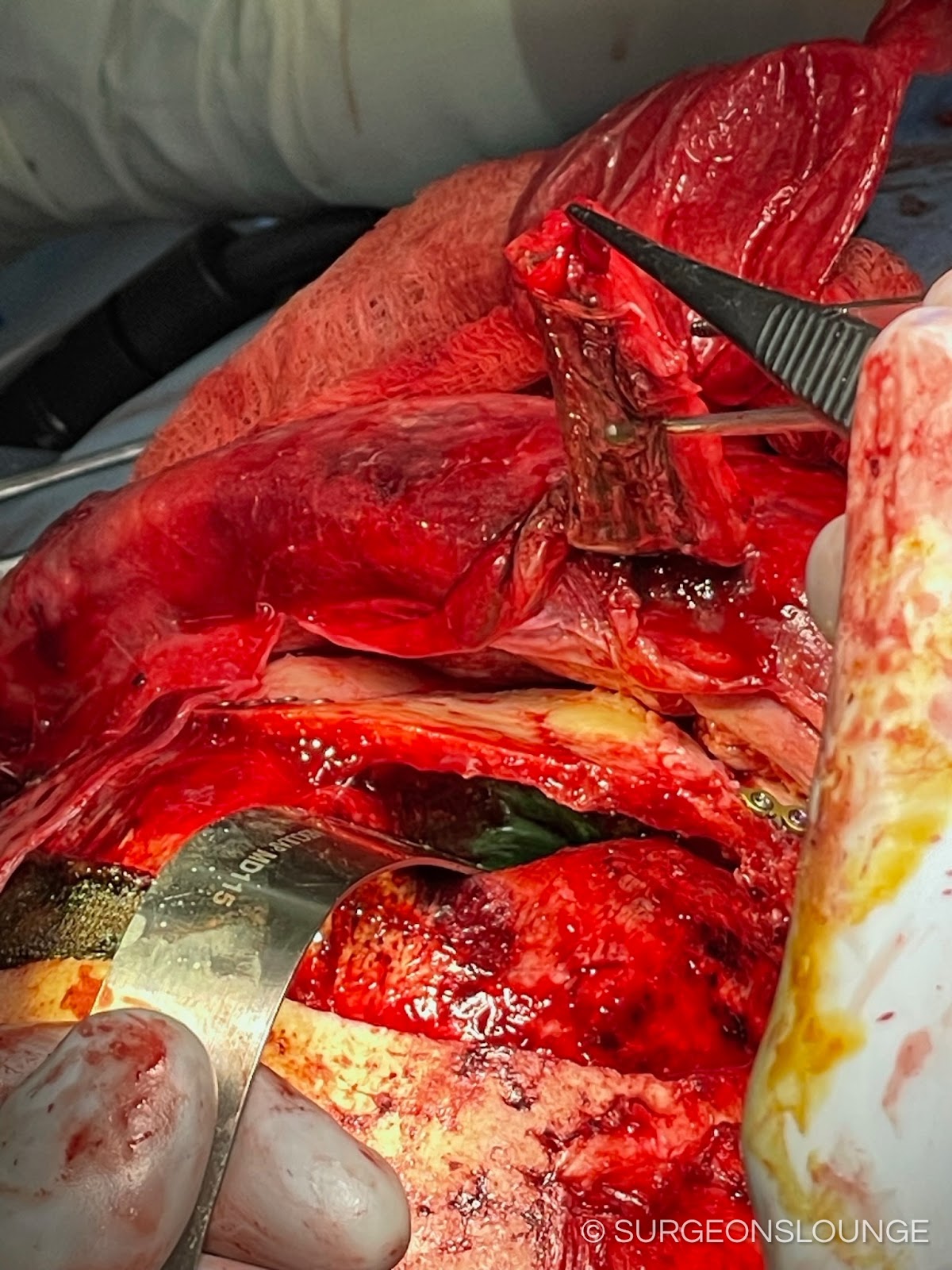
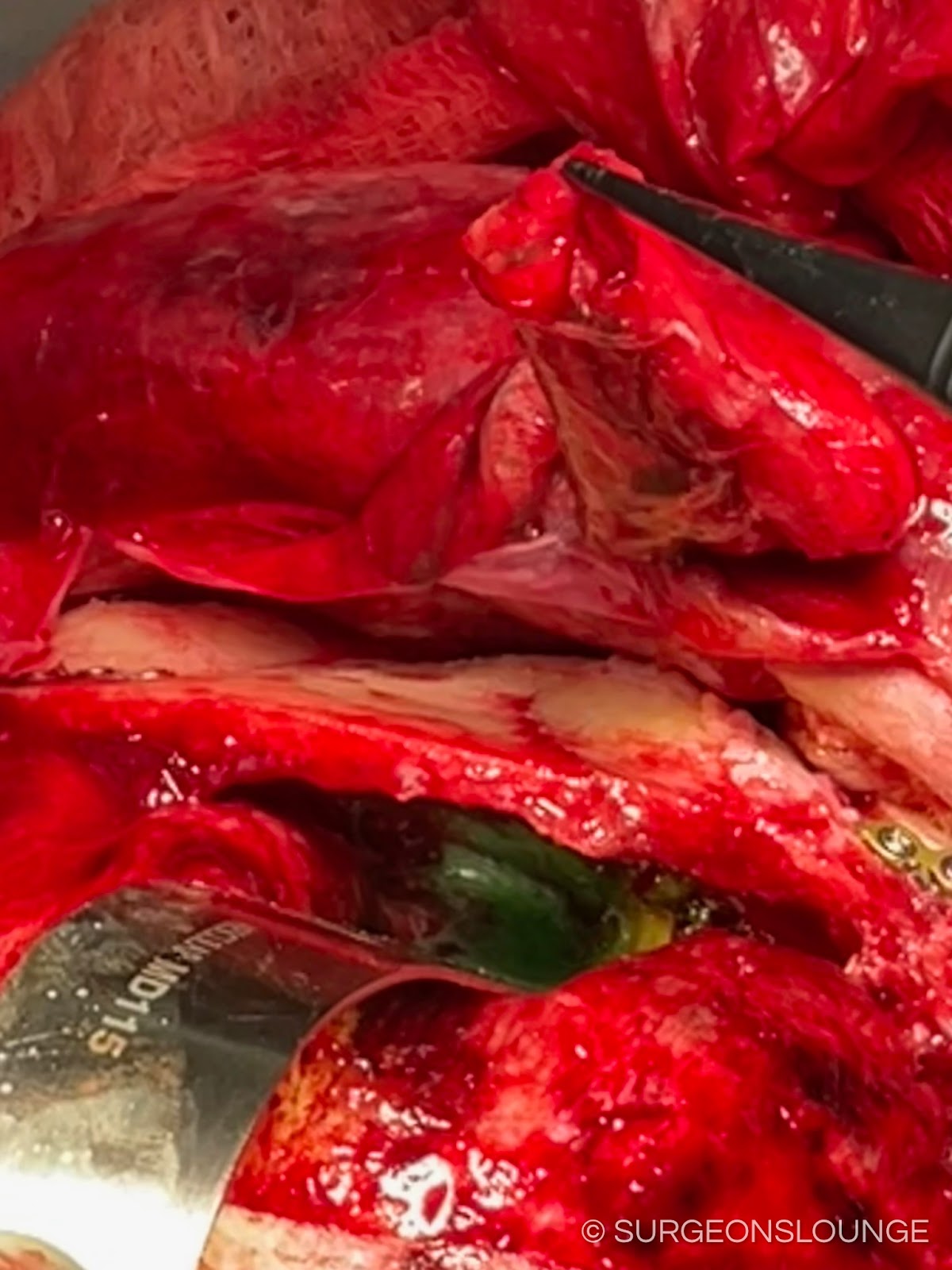
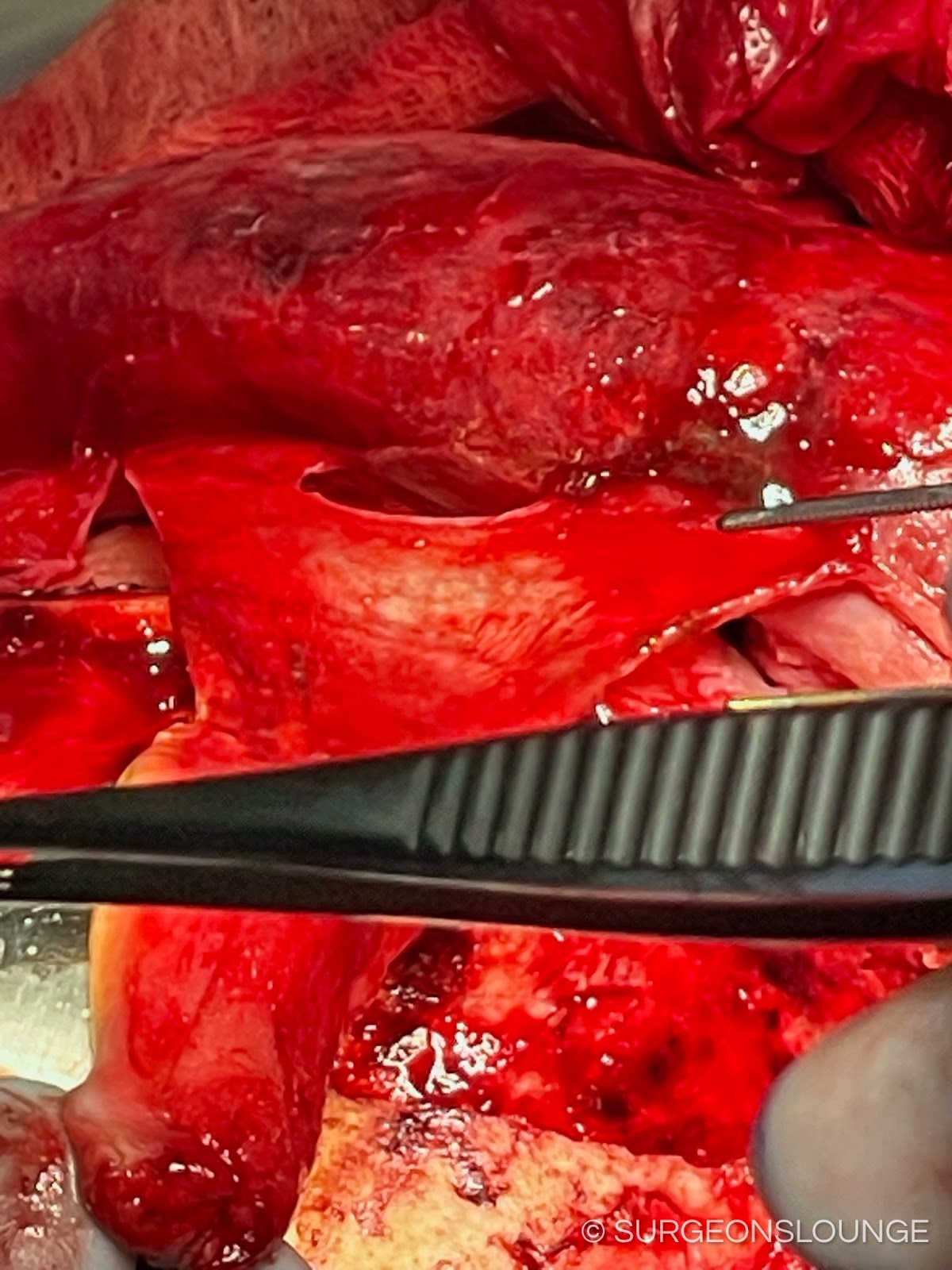
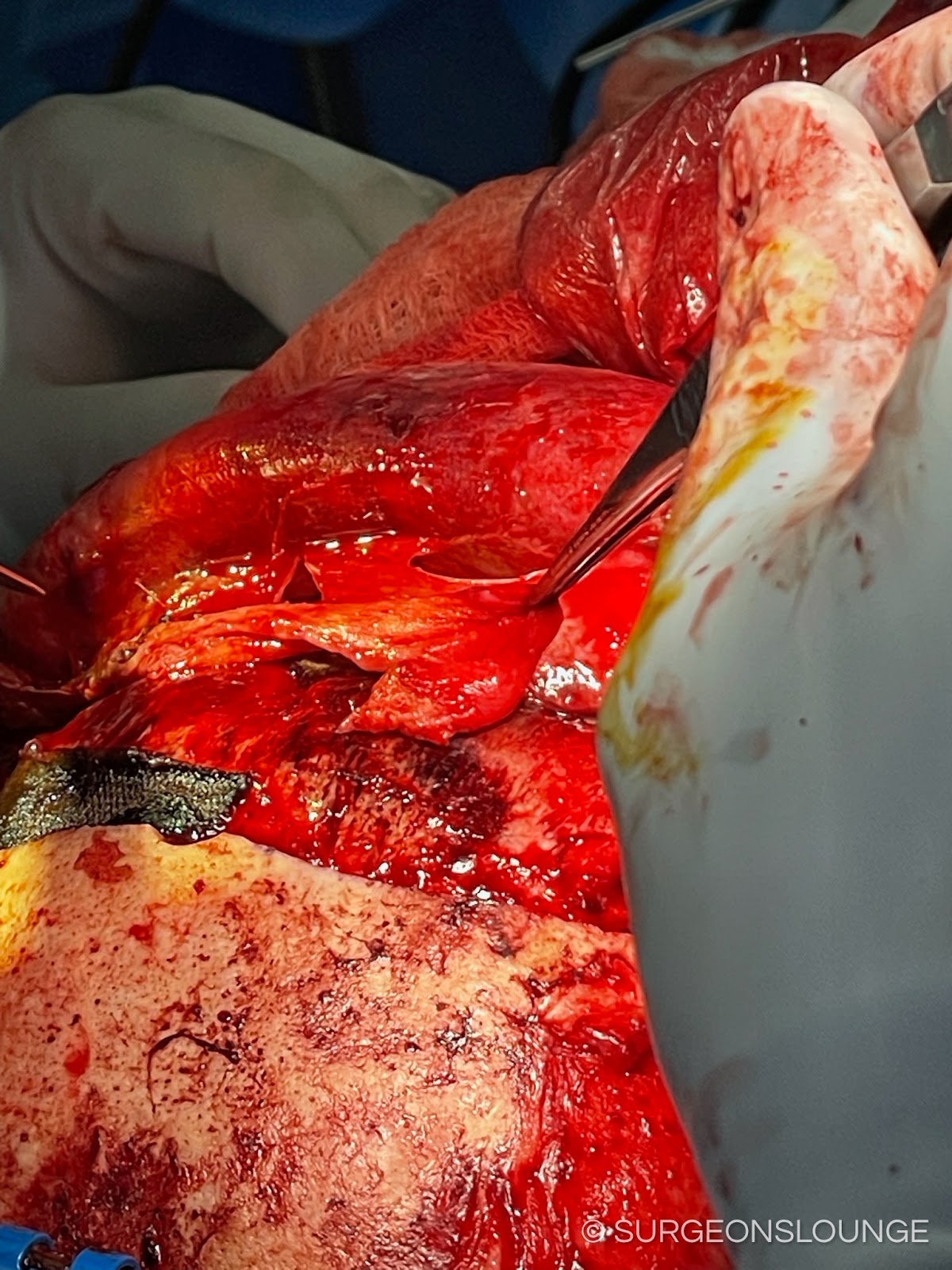
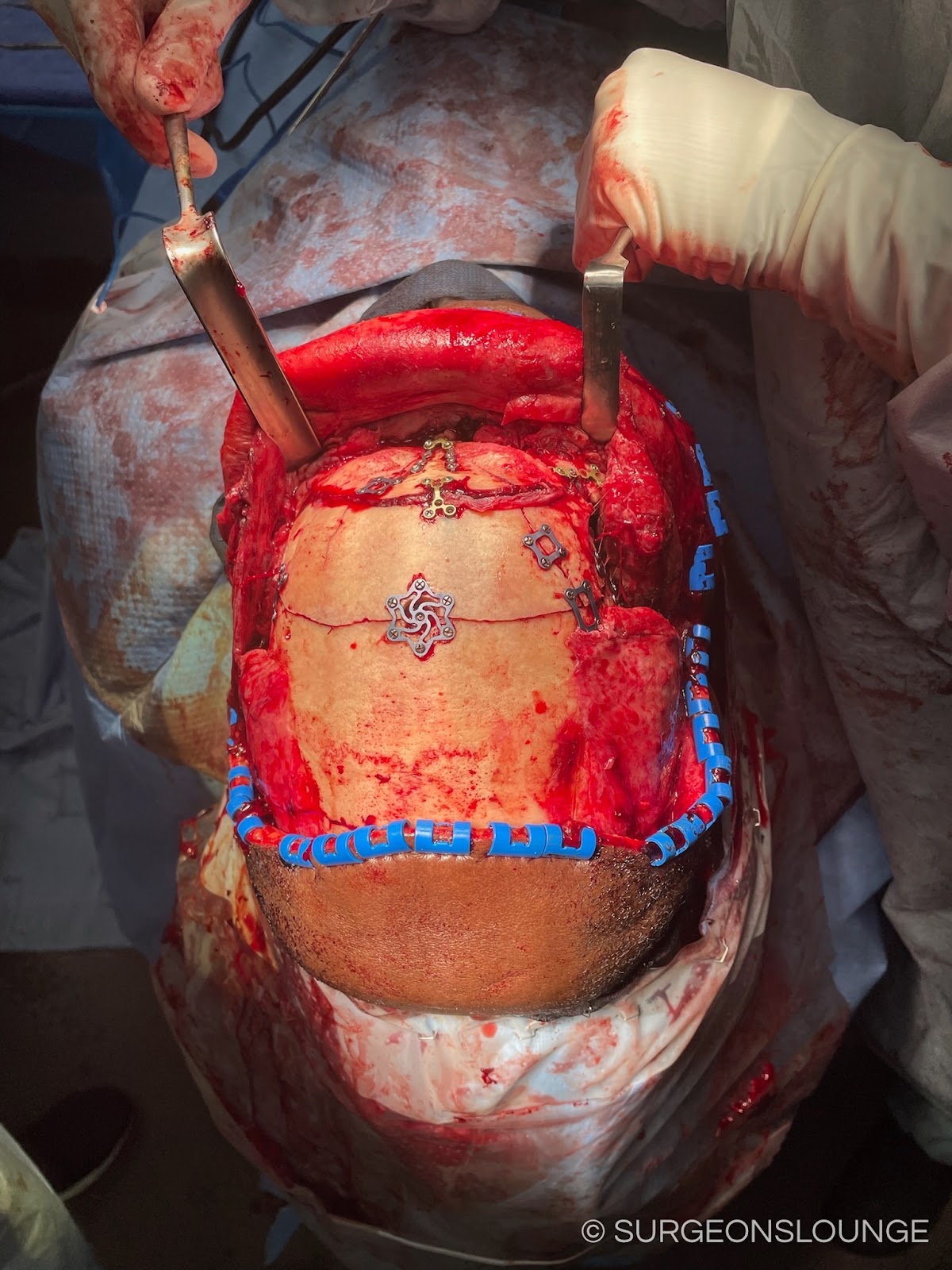
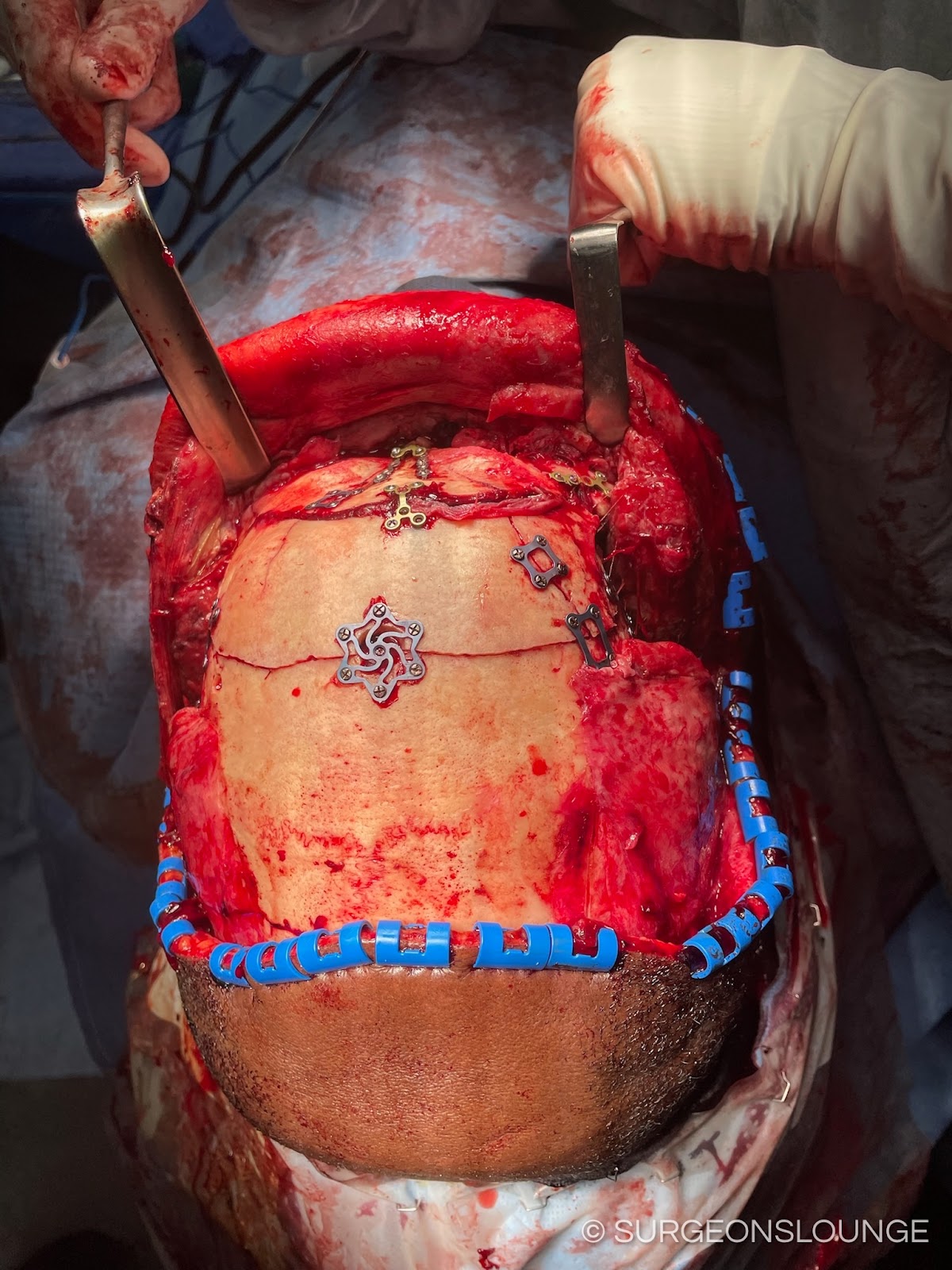
At the area of the temporal crest curved stats and a Kelly hemostat were used to g into a smbgaleal pocket. A bovie and bipolar were used to control any bleeders along the incision site. A #9 subperiosteal was used to create a pocket in a subperiosteal plane using a lap to create tension. In the area of the temporal crest dissect in a sub tempo parietal plane stying superficial to the superficial layer of the deep cervical fascia. Palpate the superior orbital rim to understand the extent of the dissection boundary.
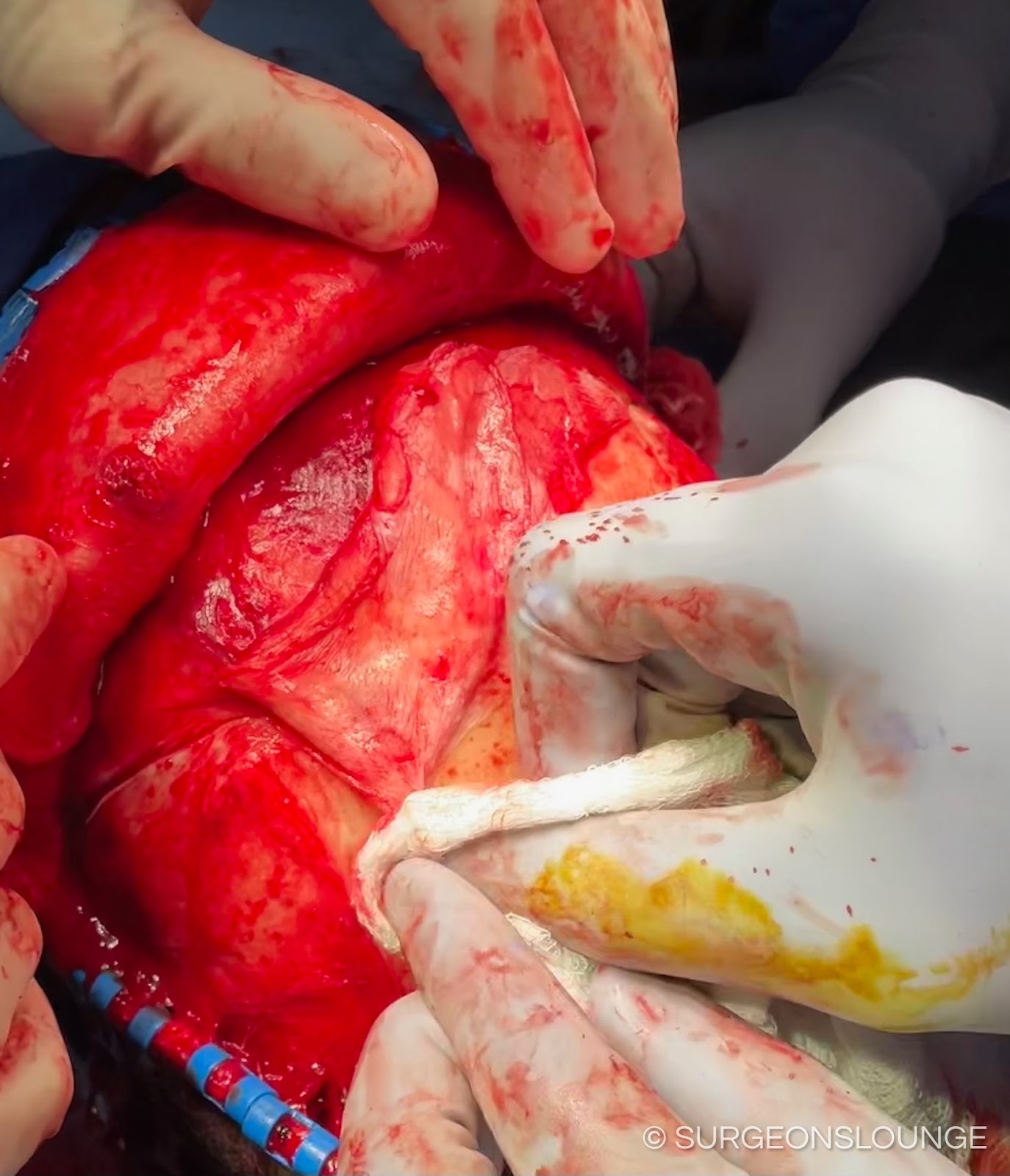
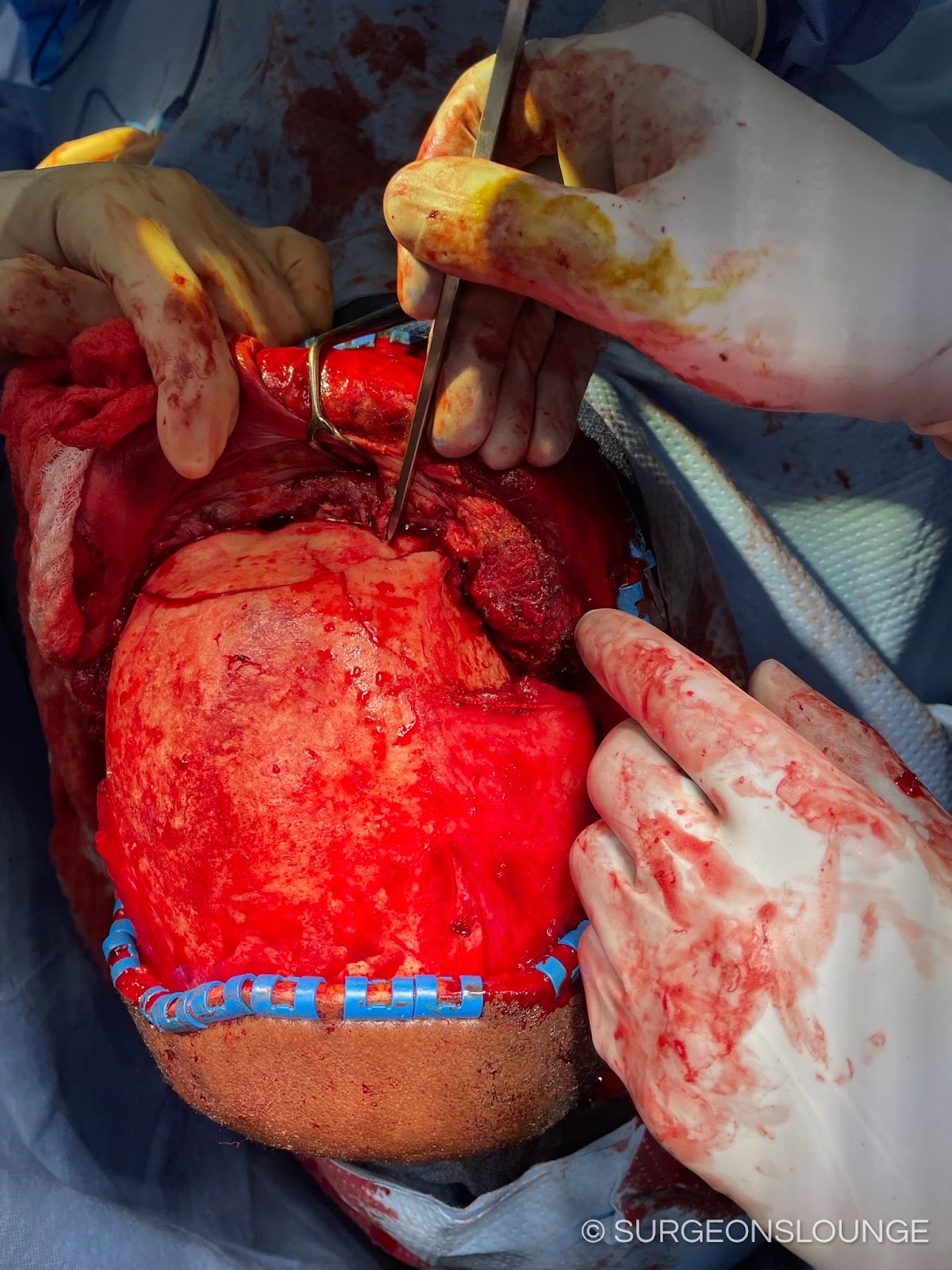
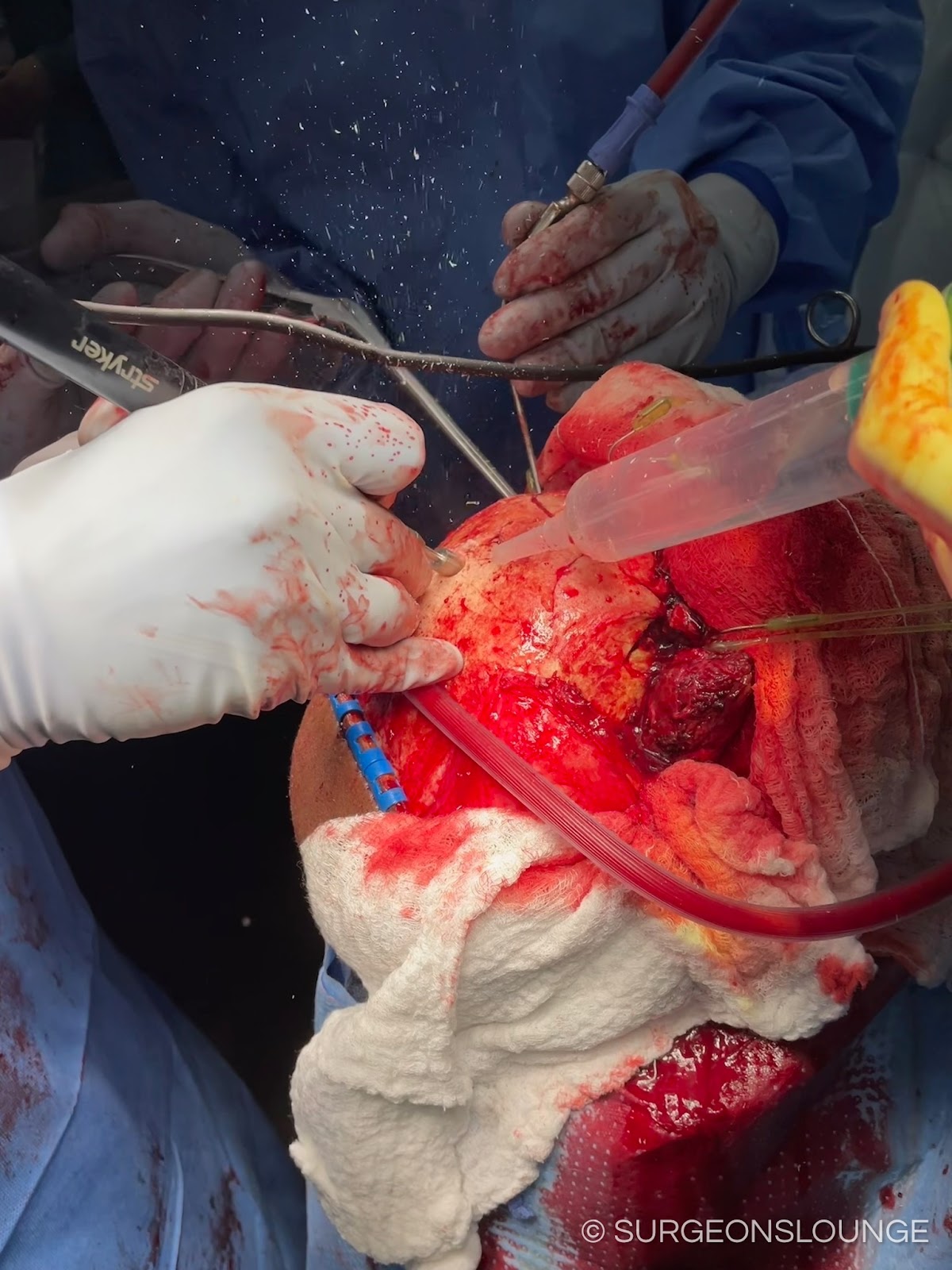
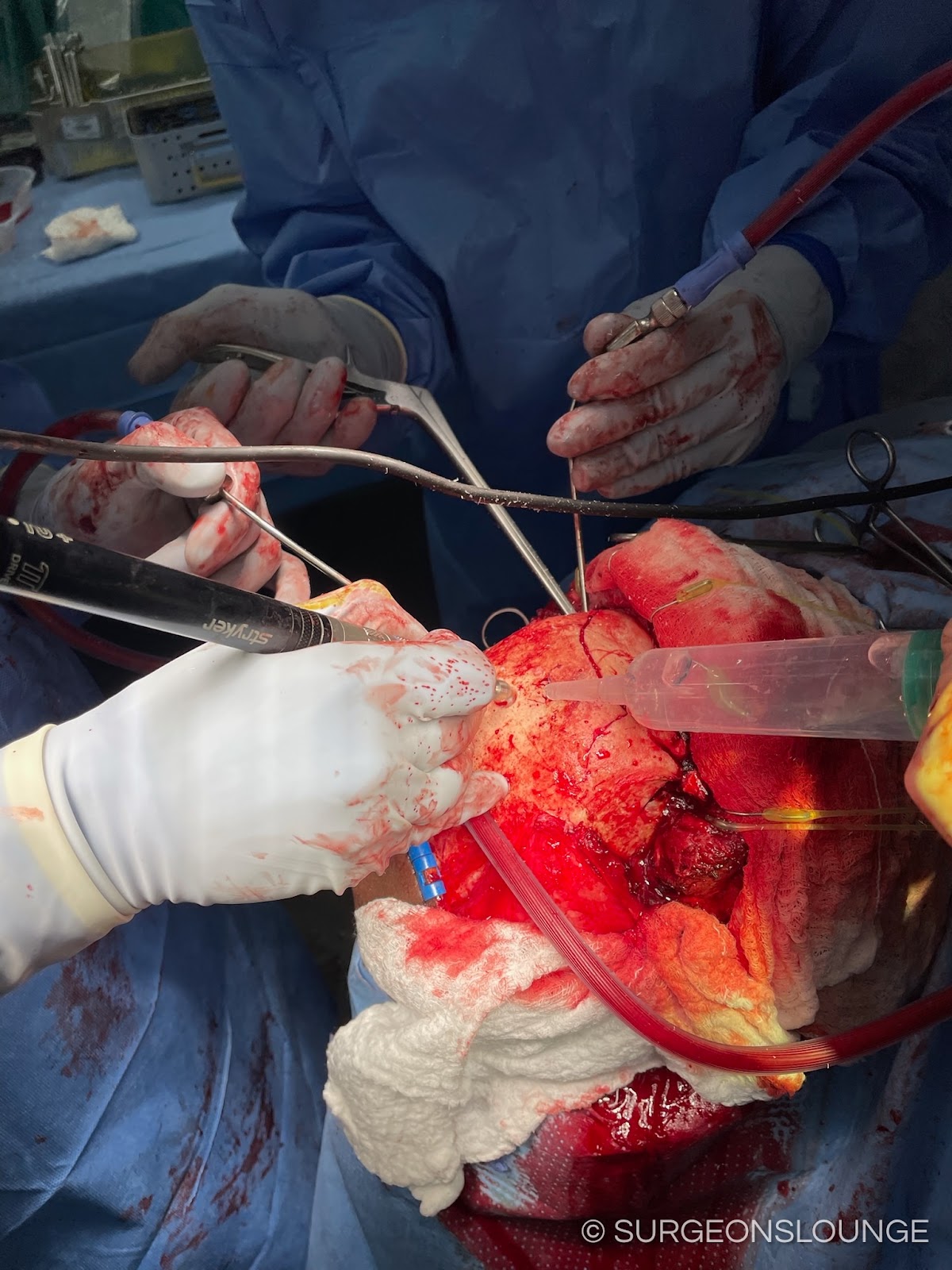
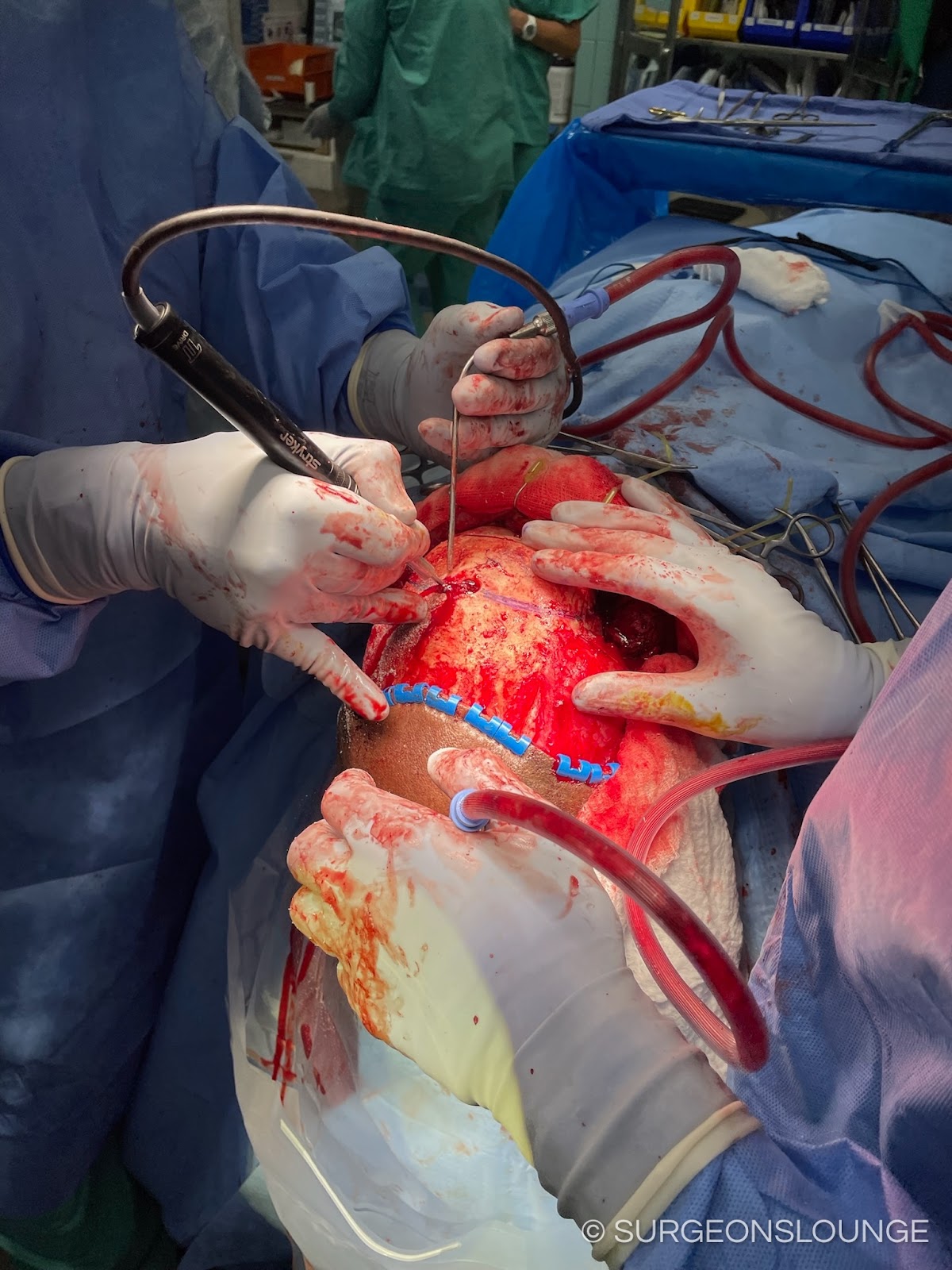
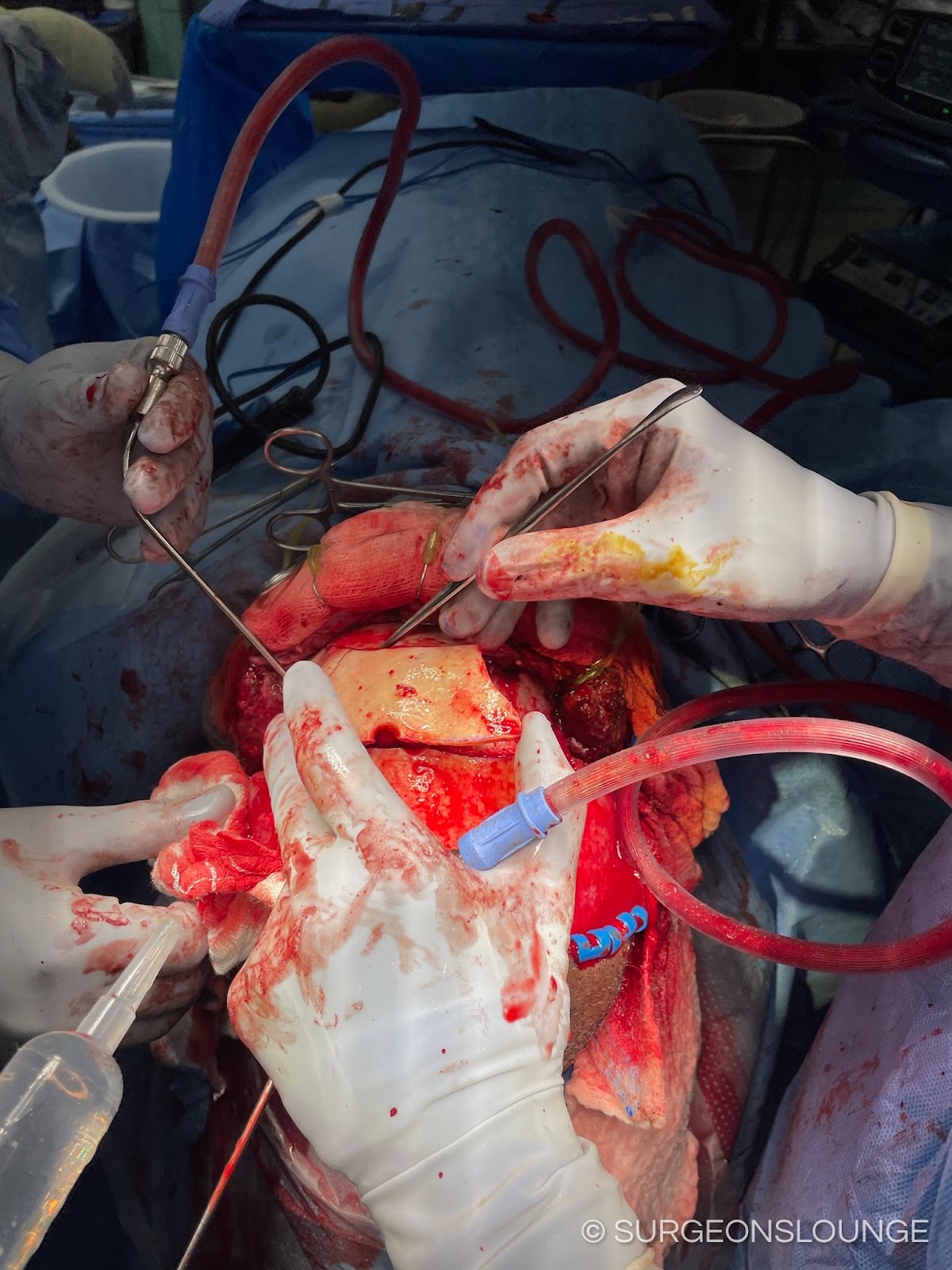
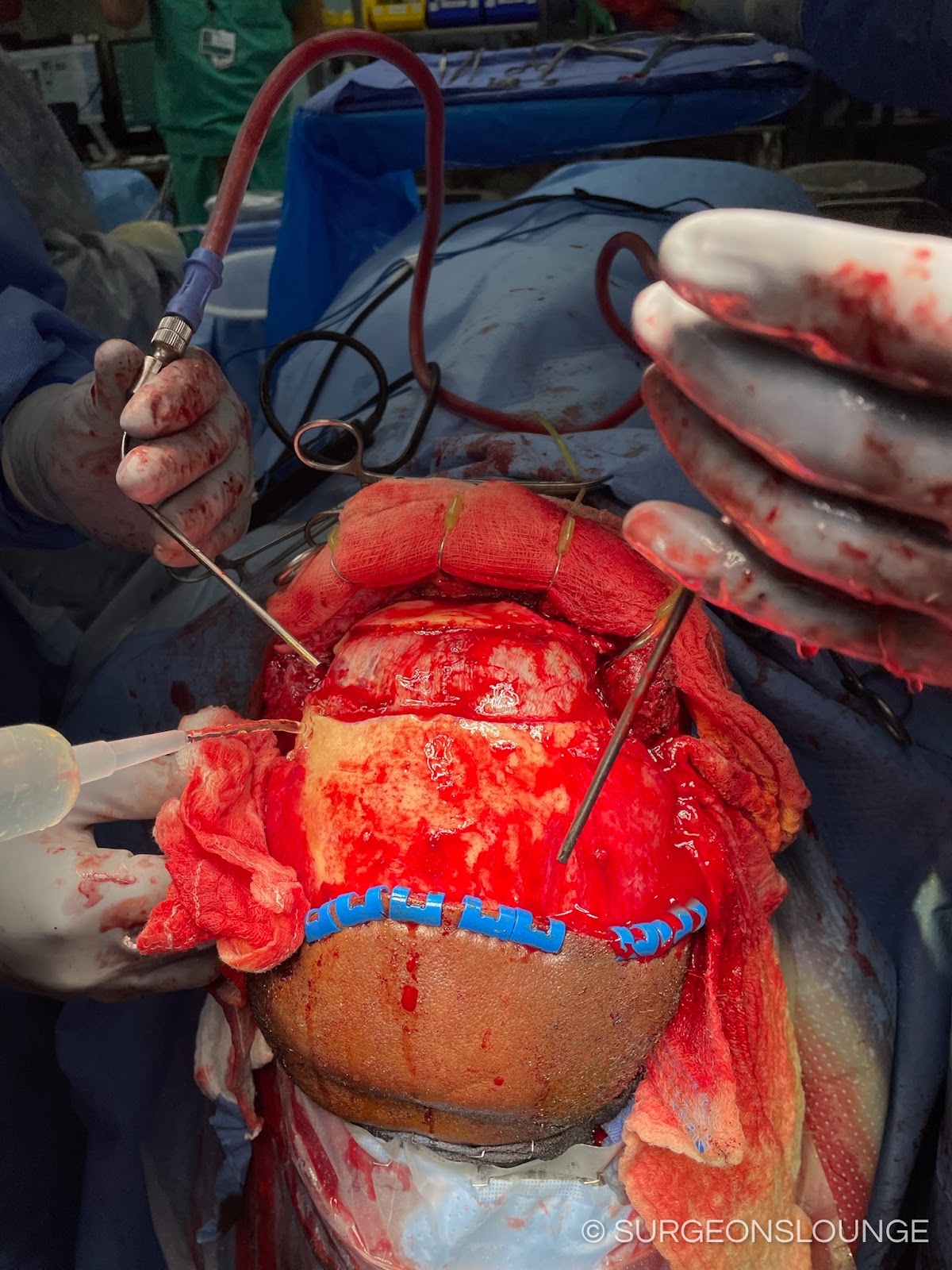
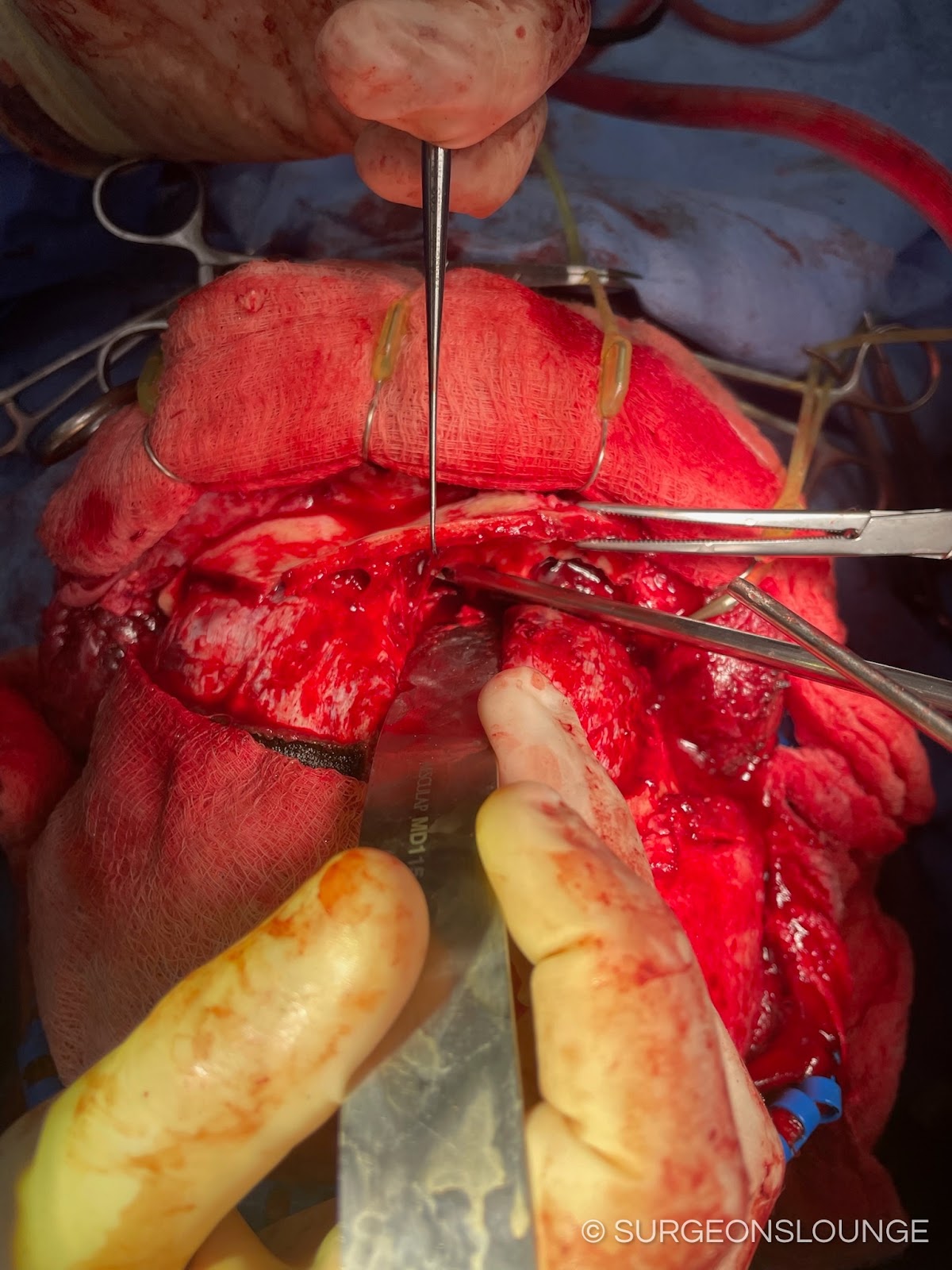
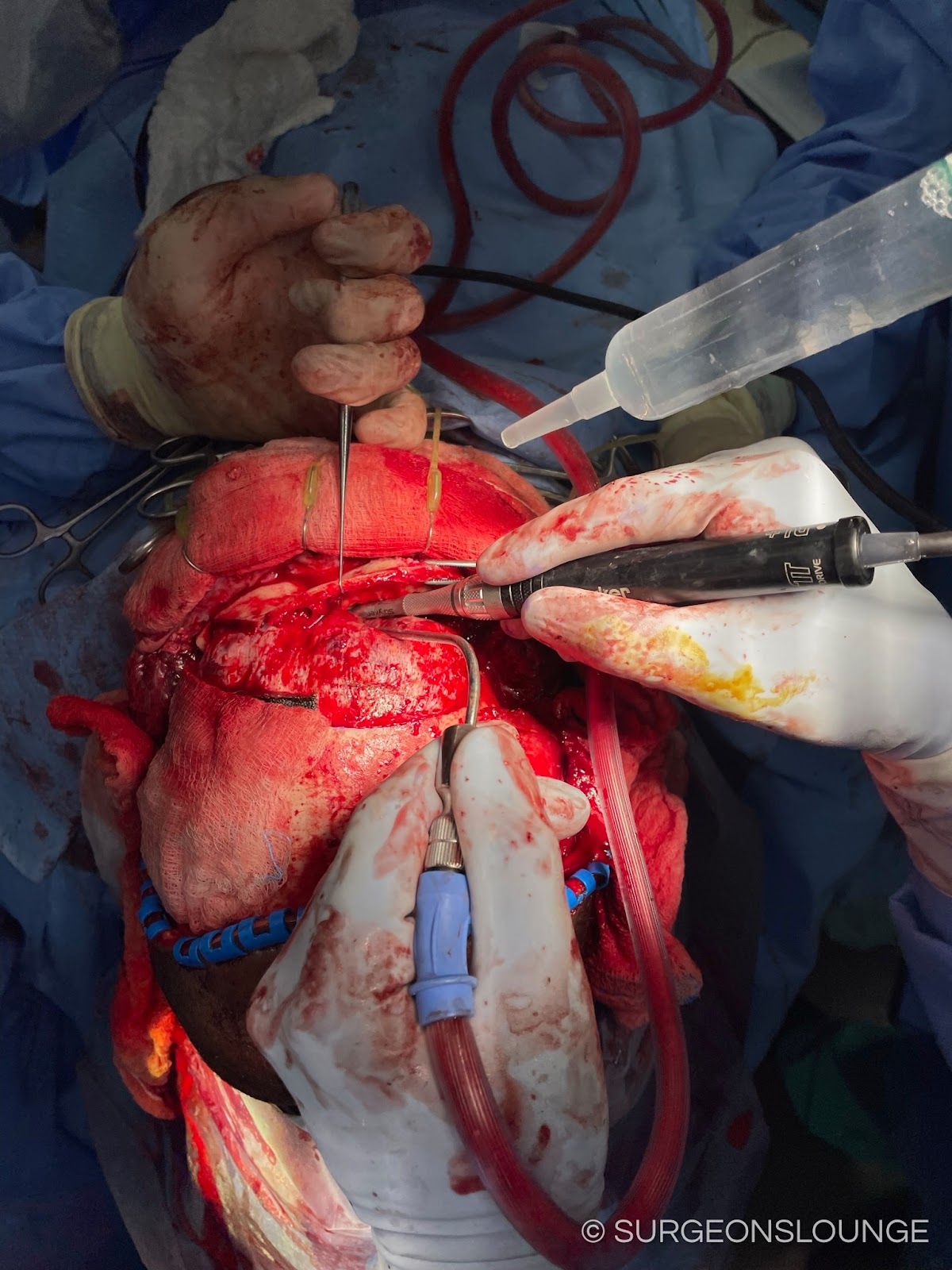
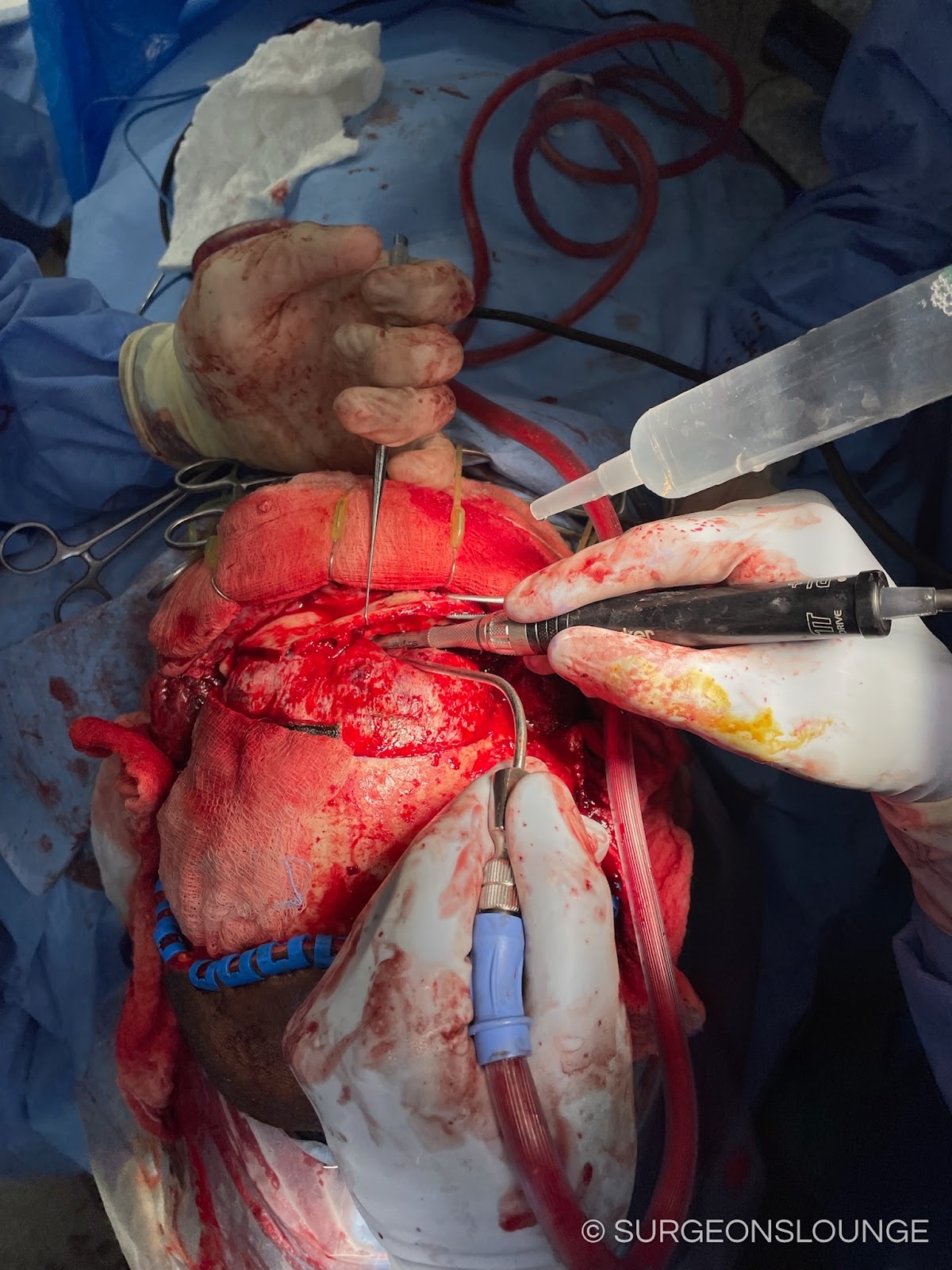
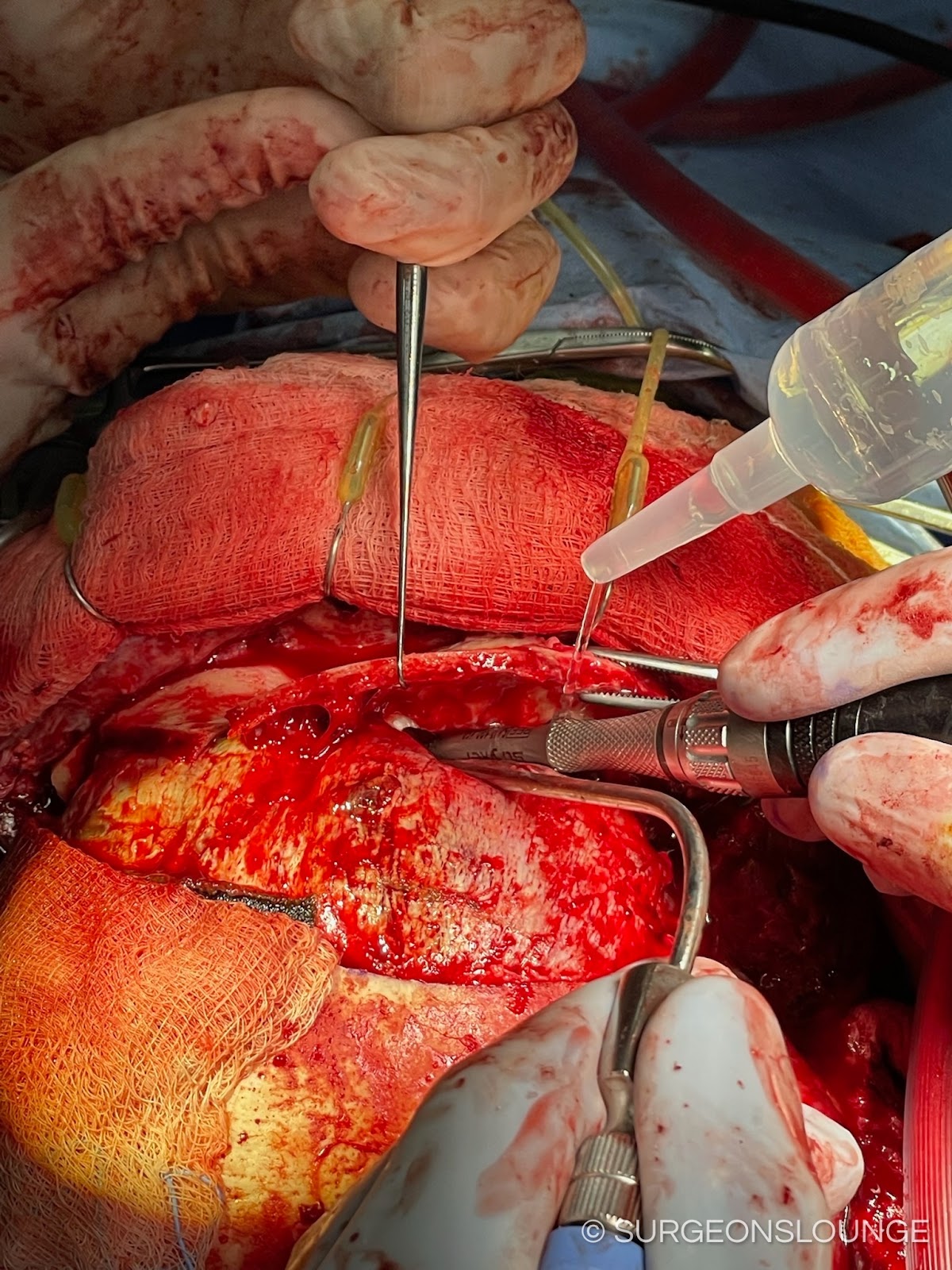
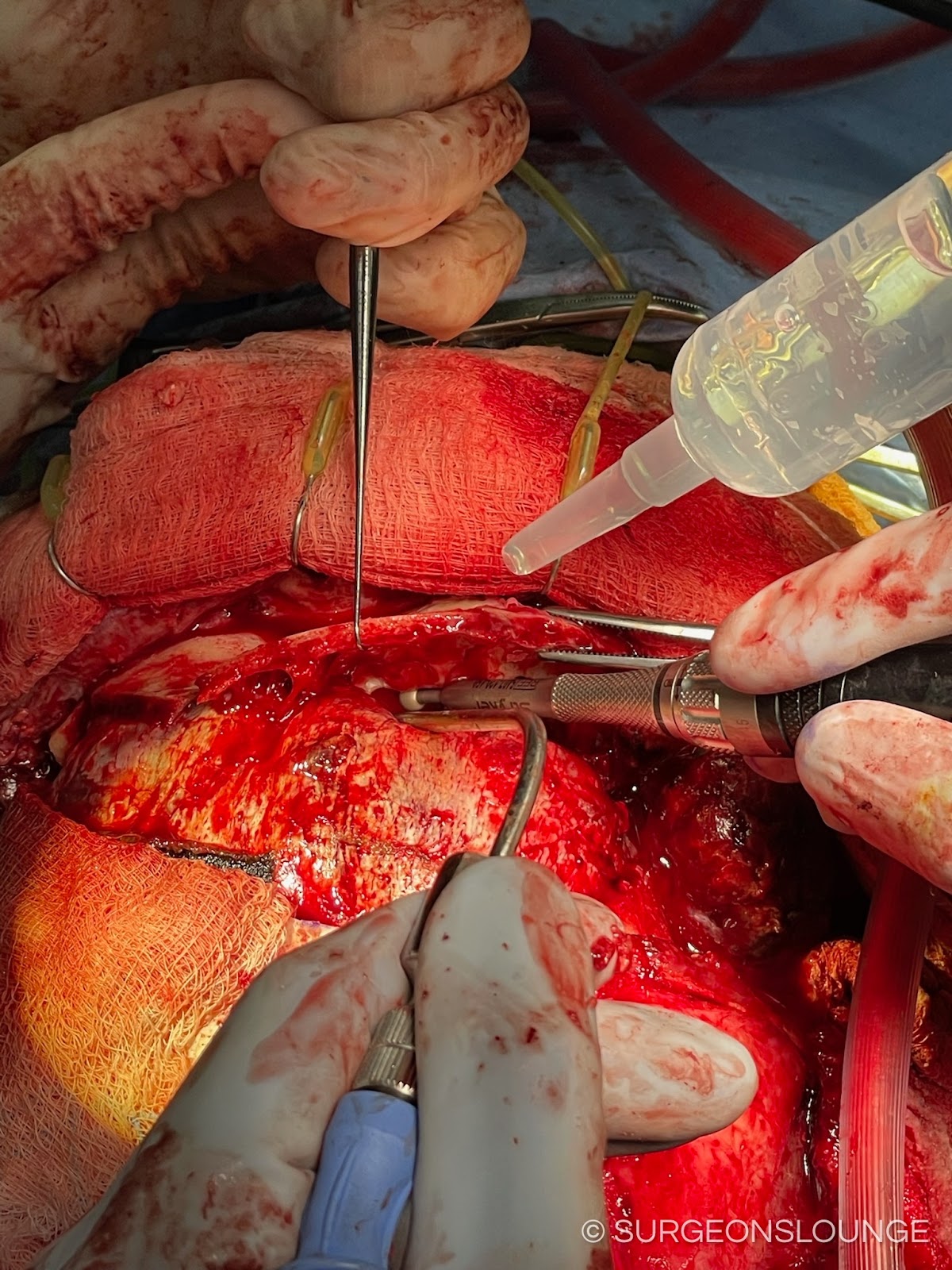
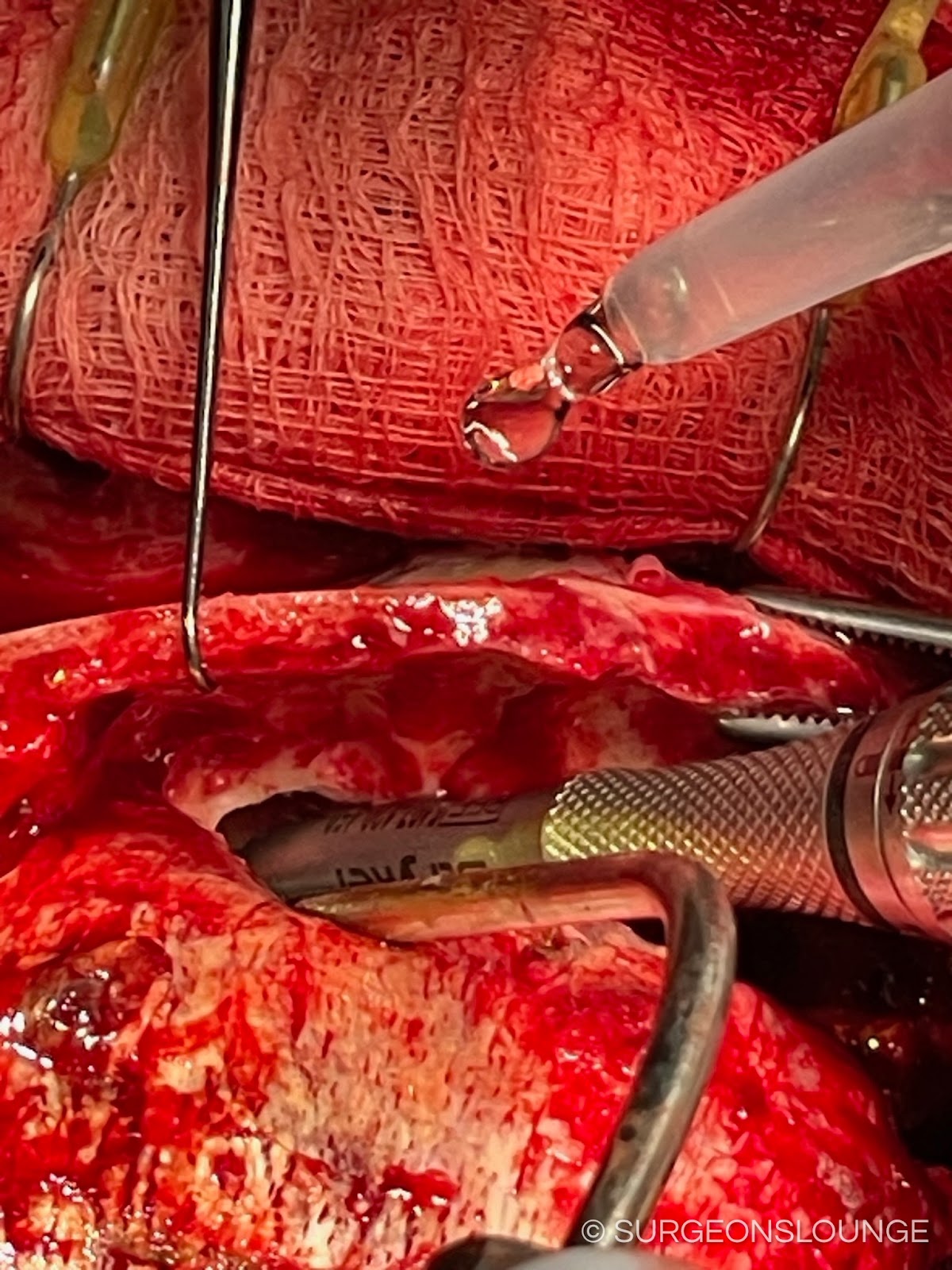
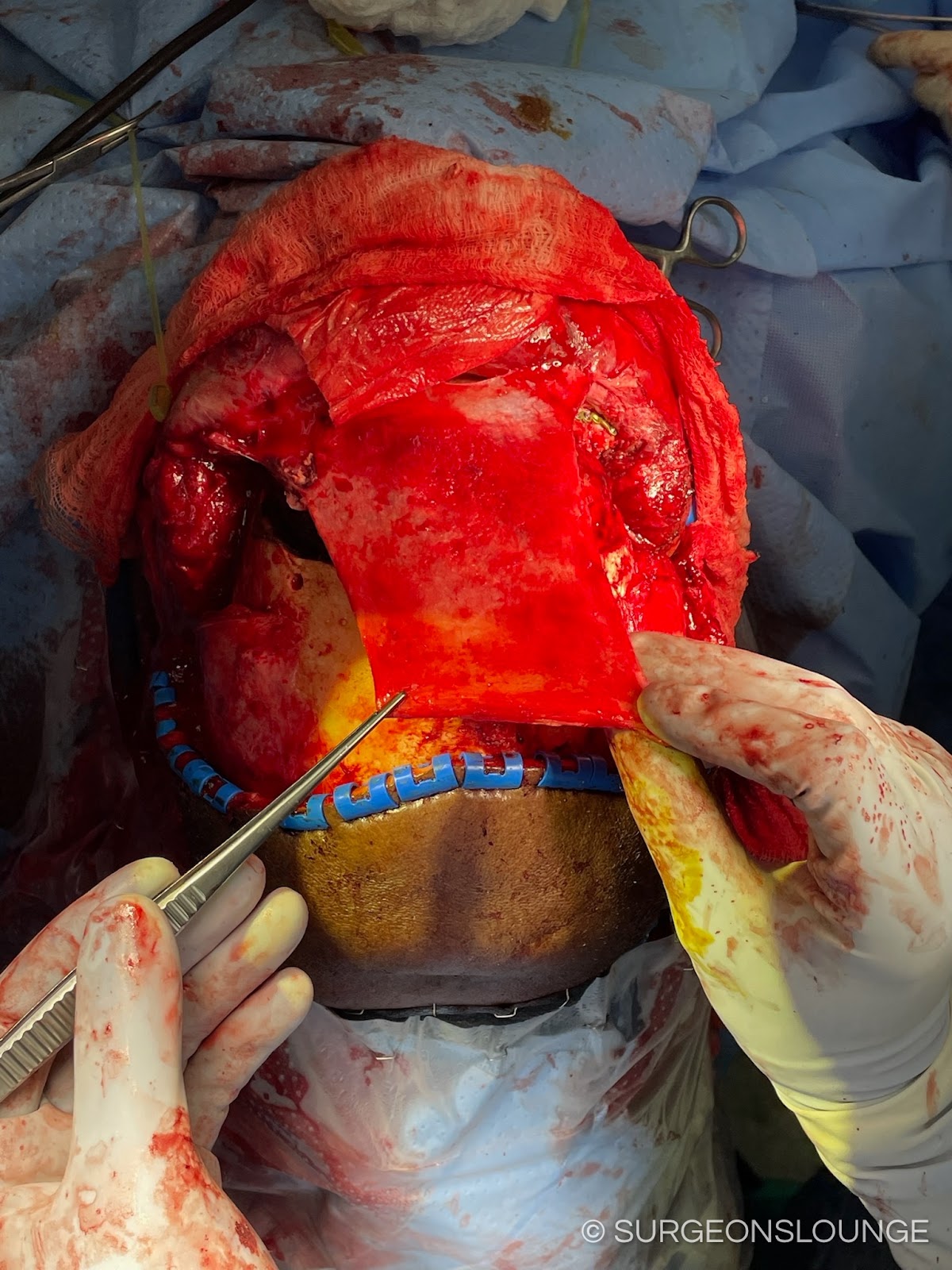
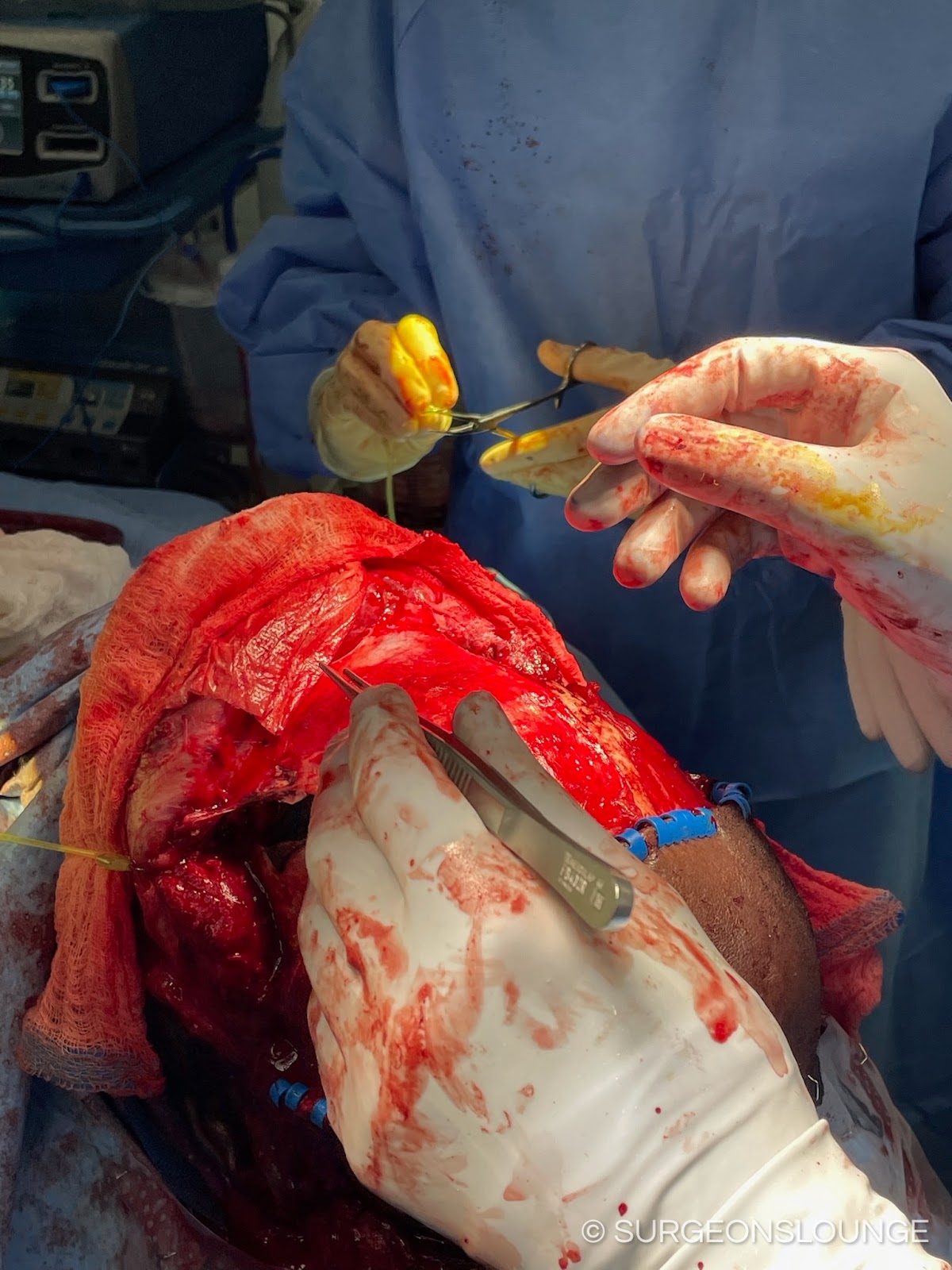
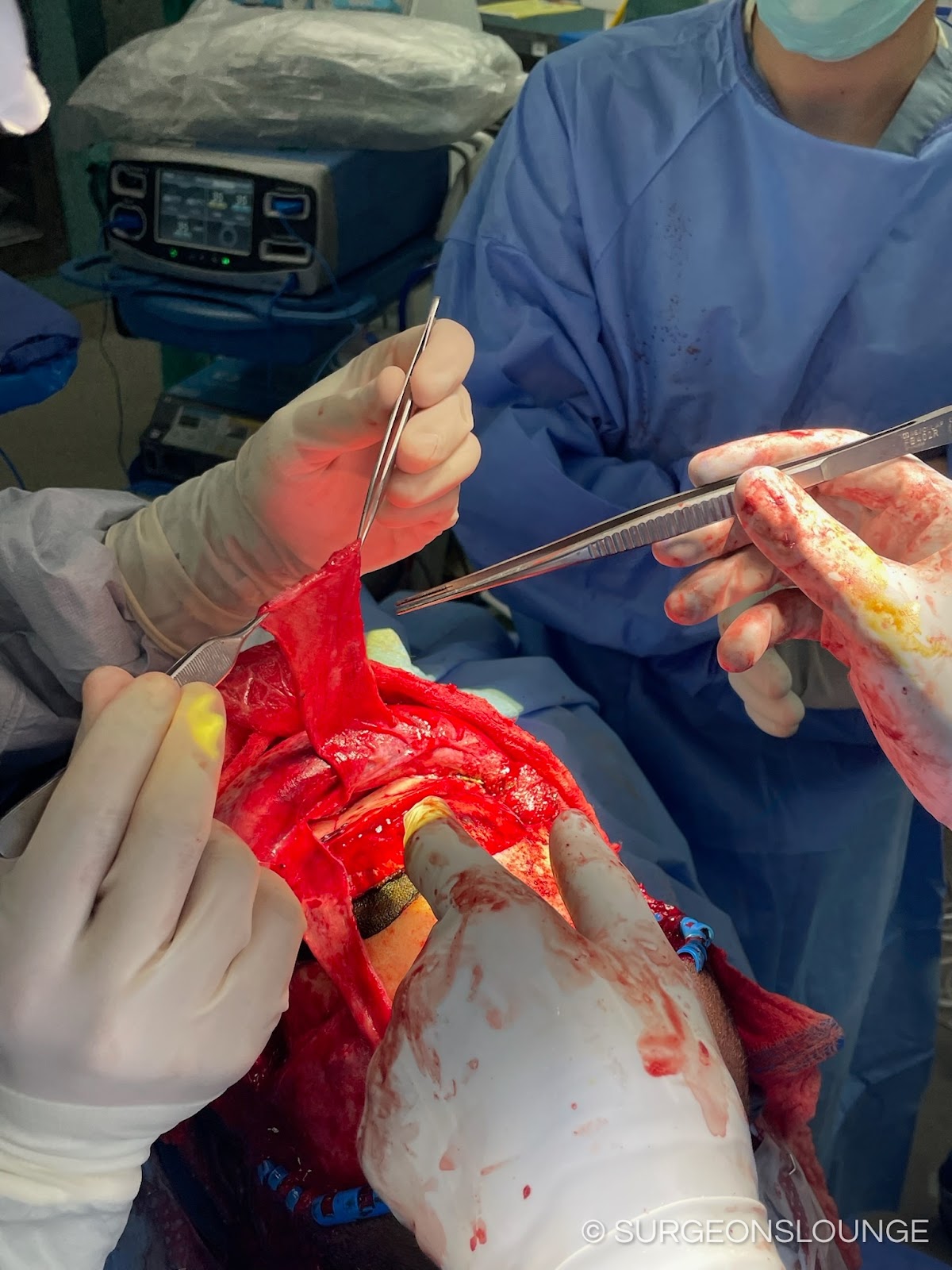
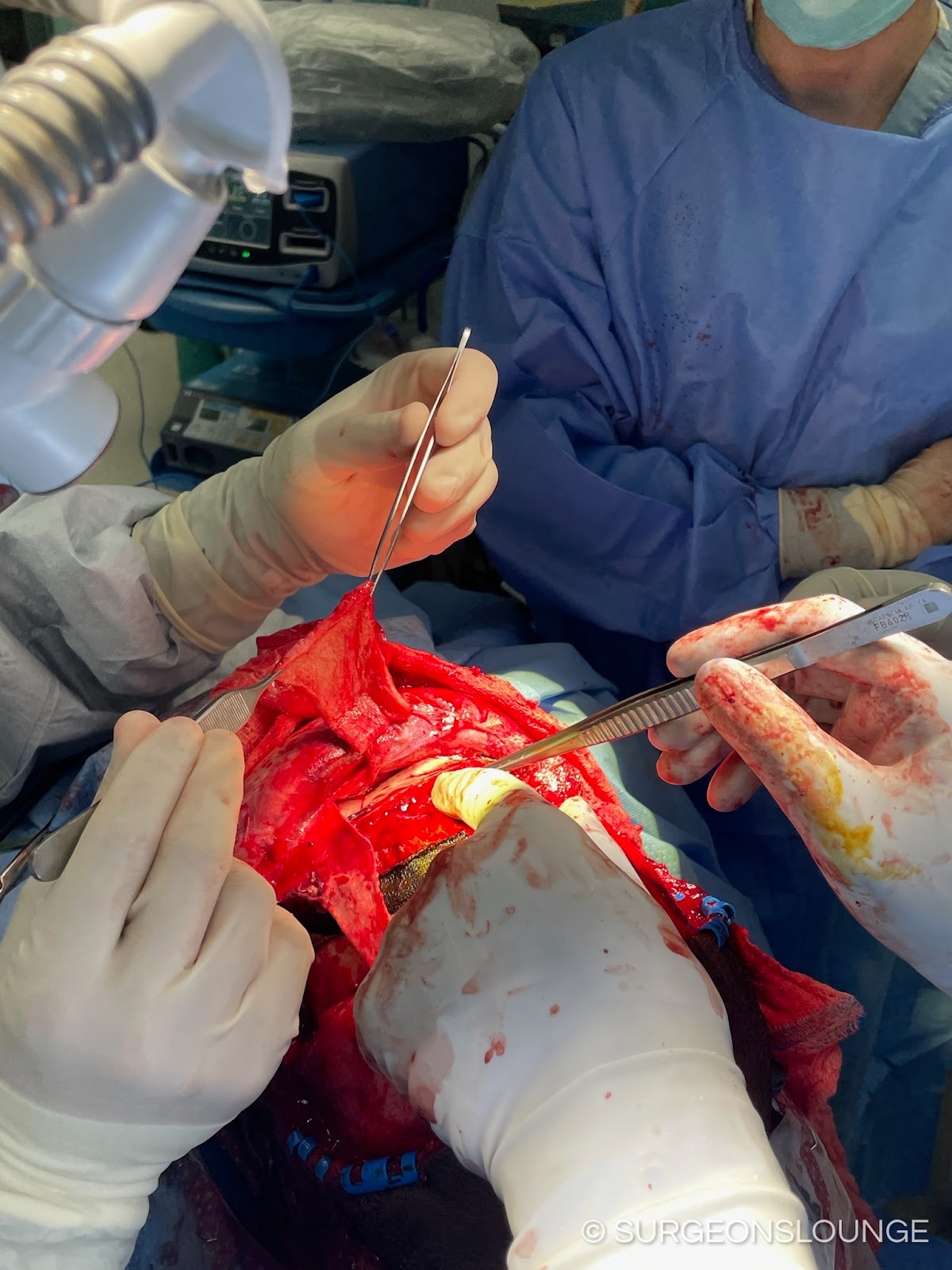
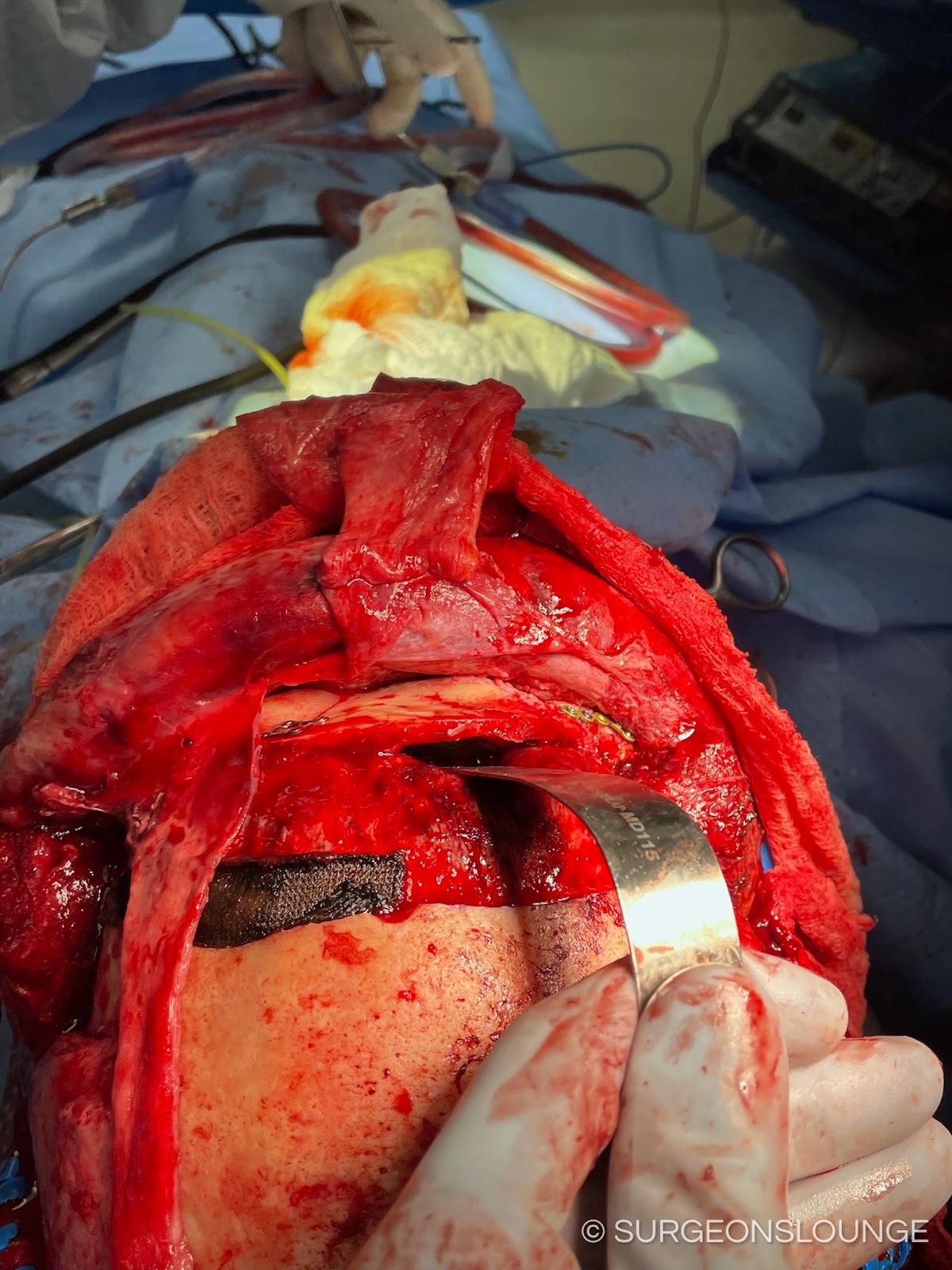
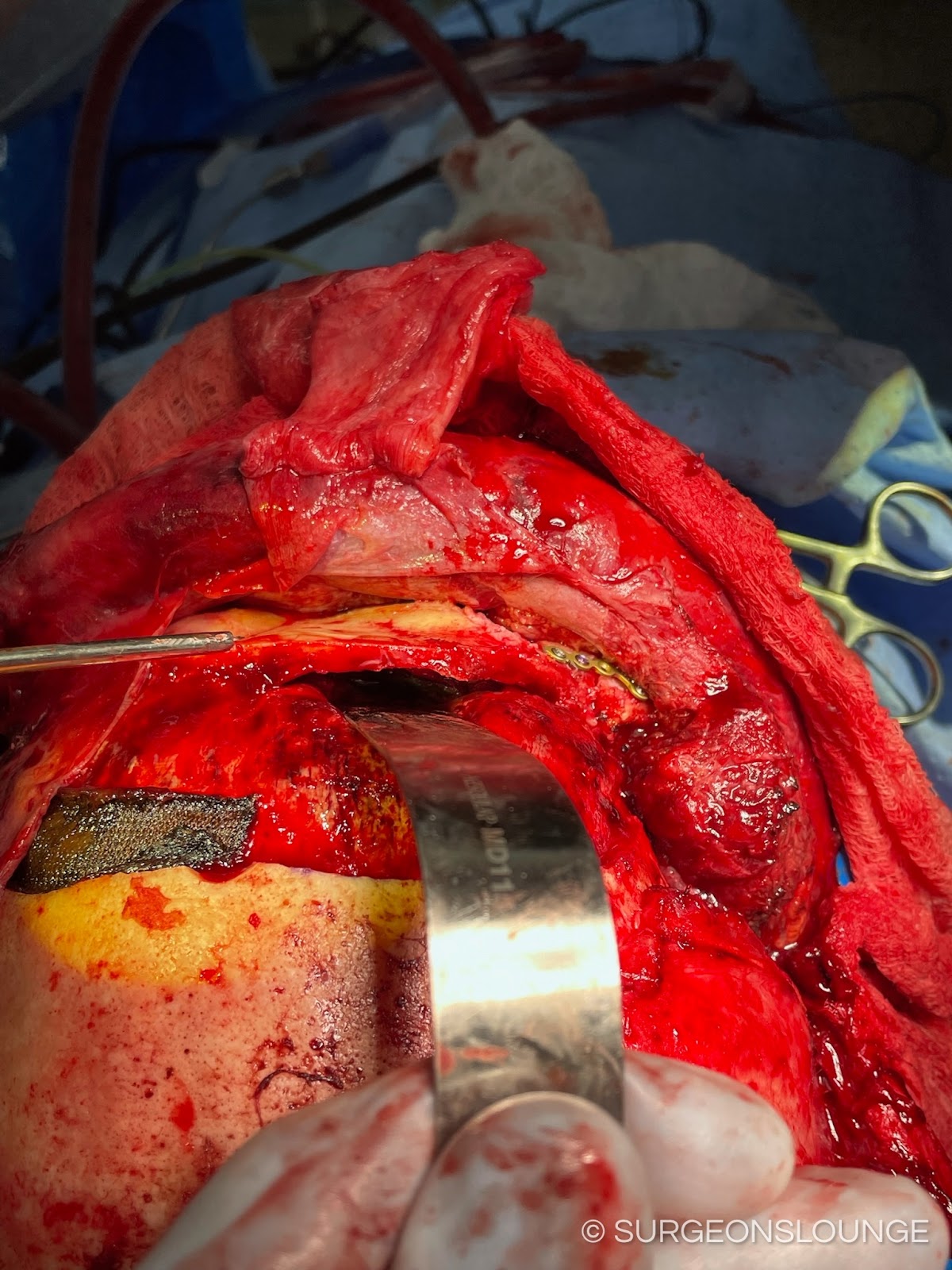
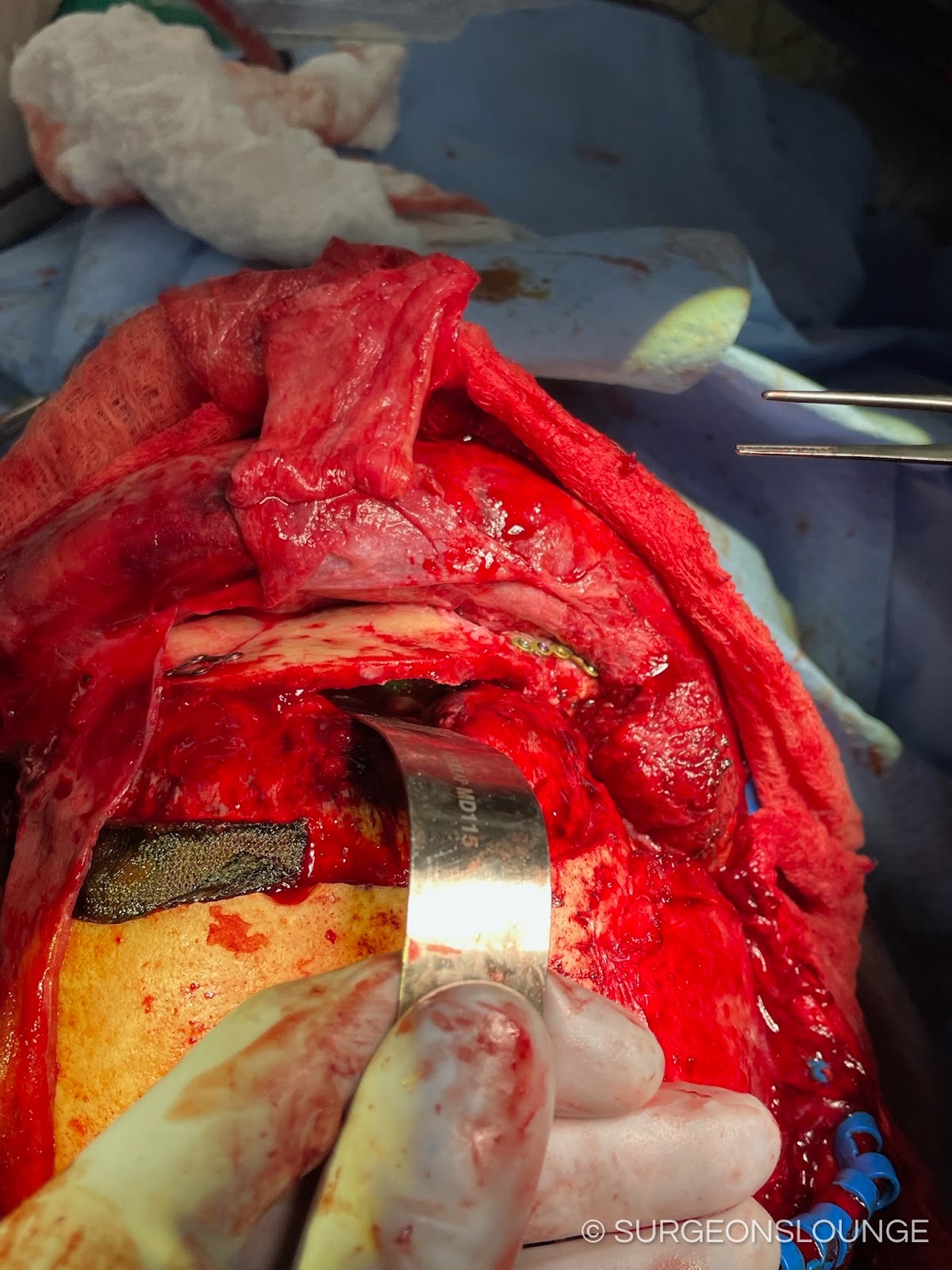
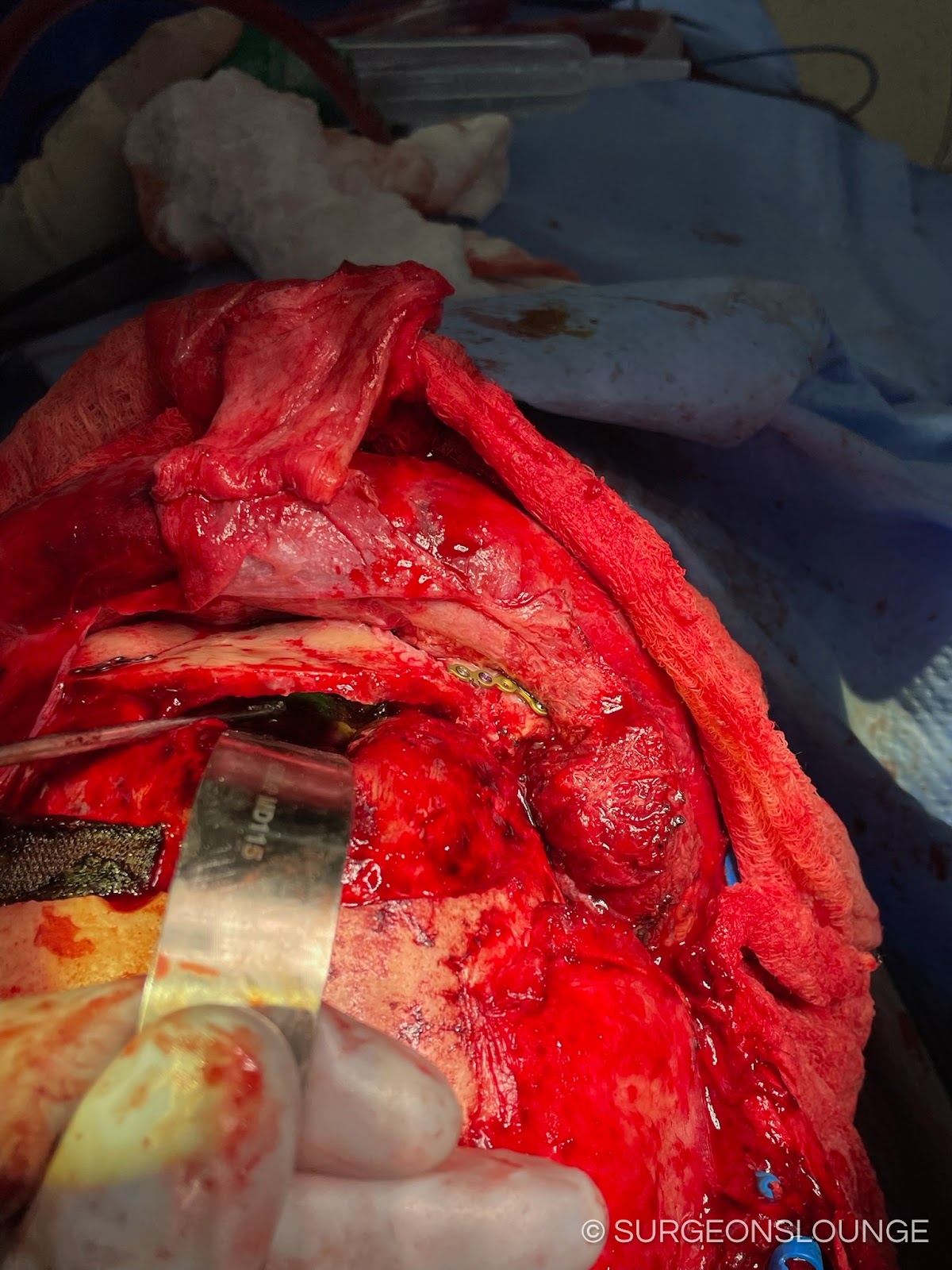
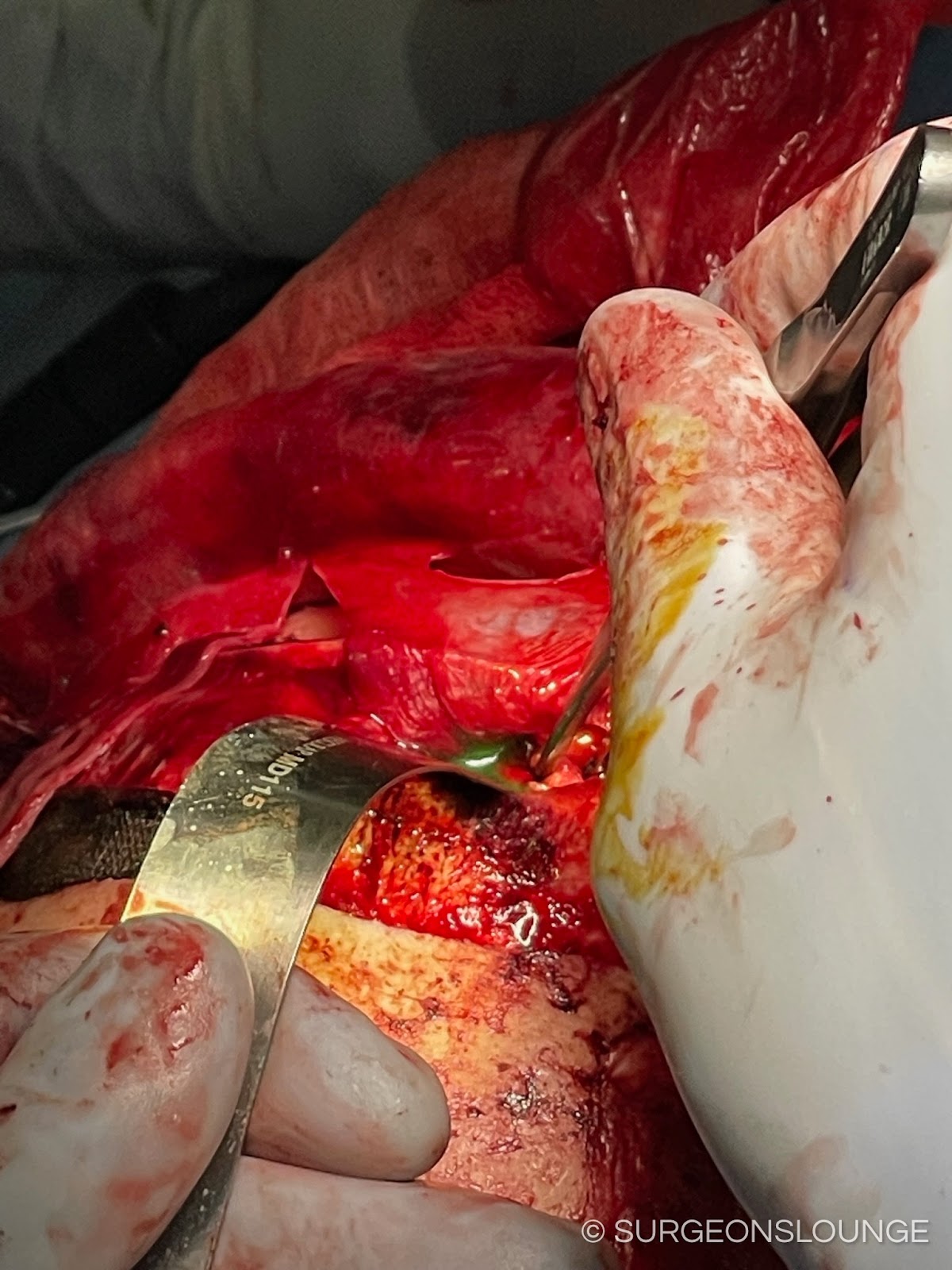
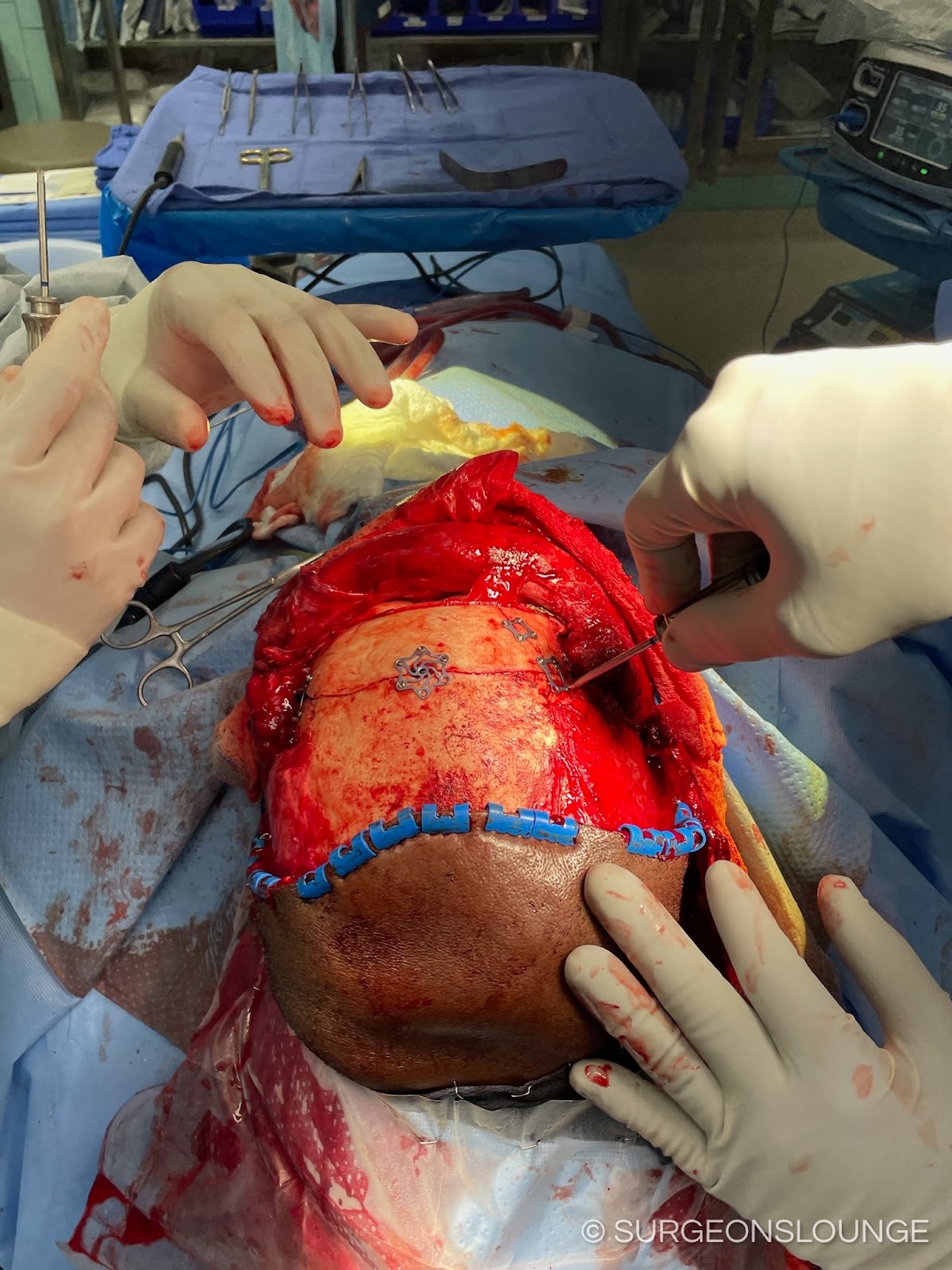
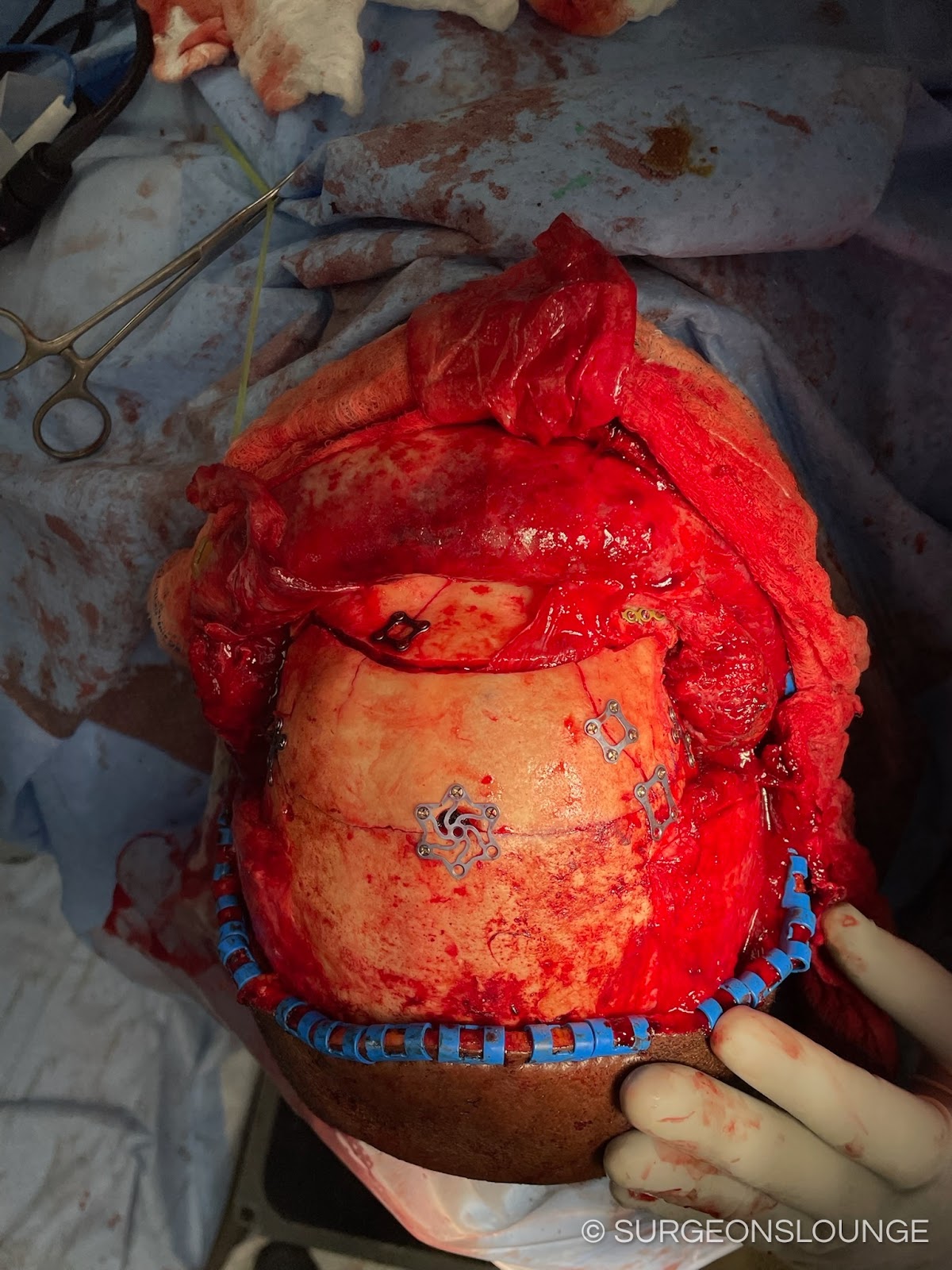
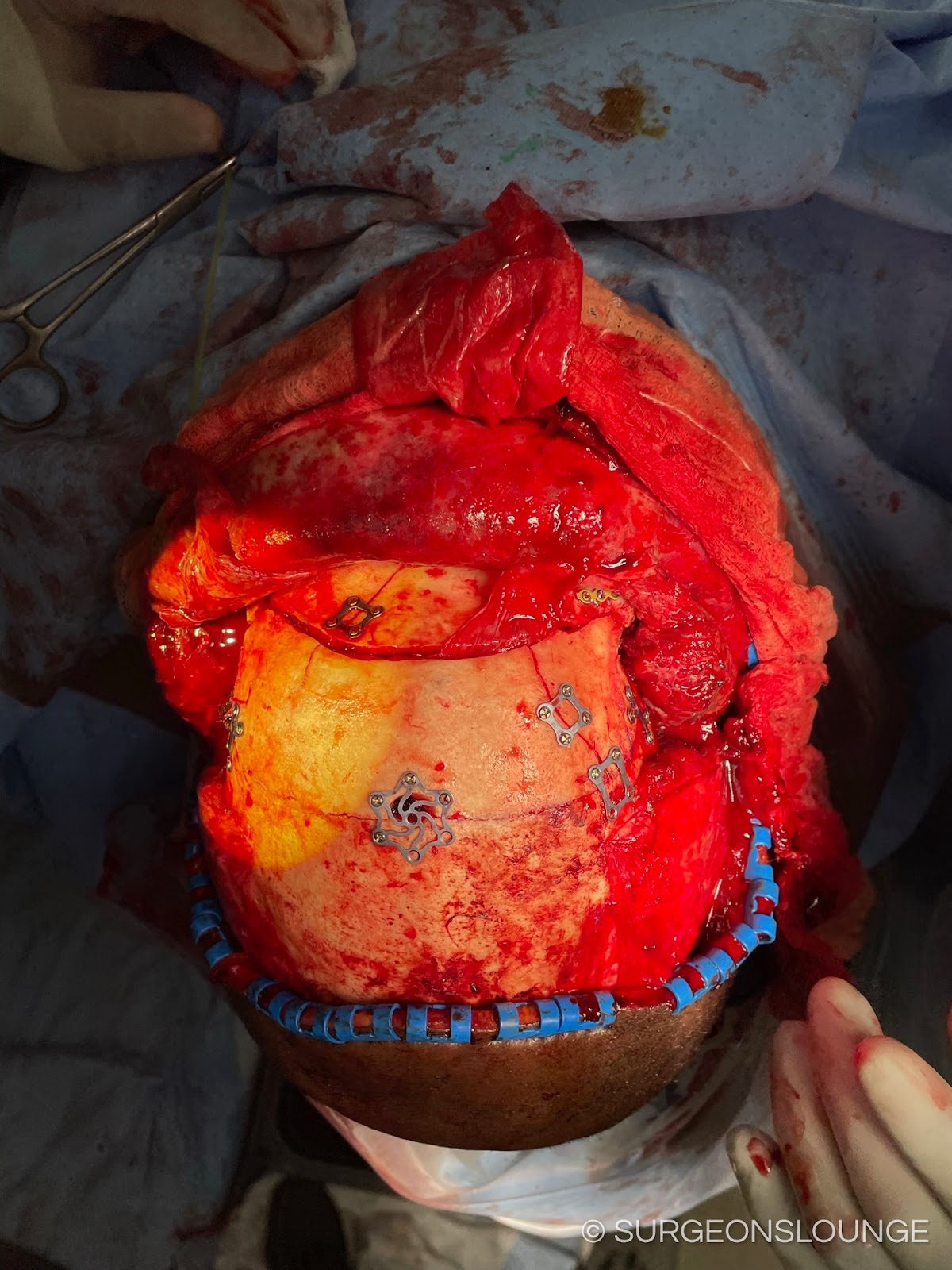
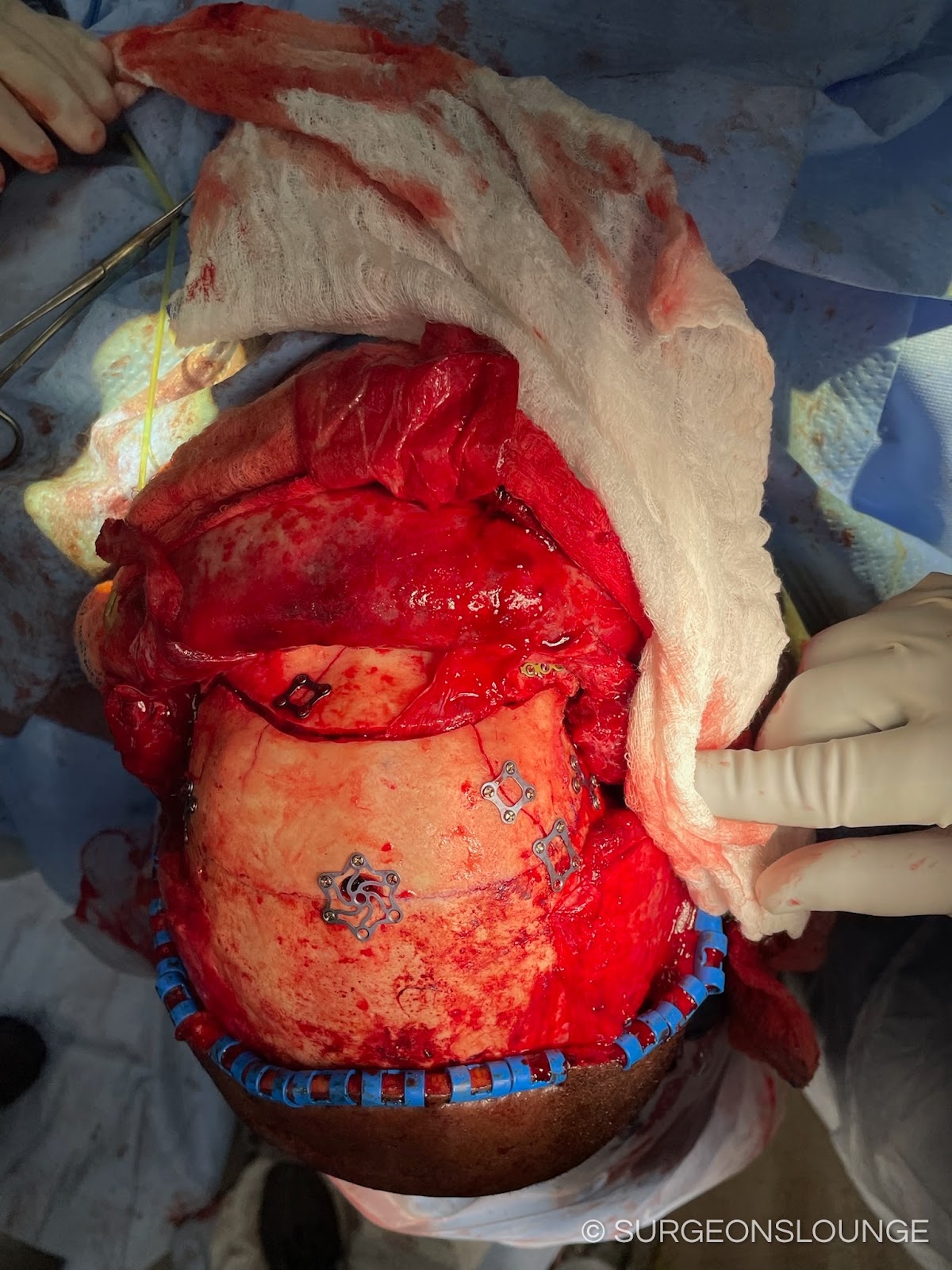
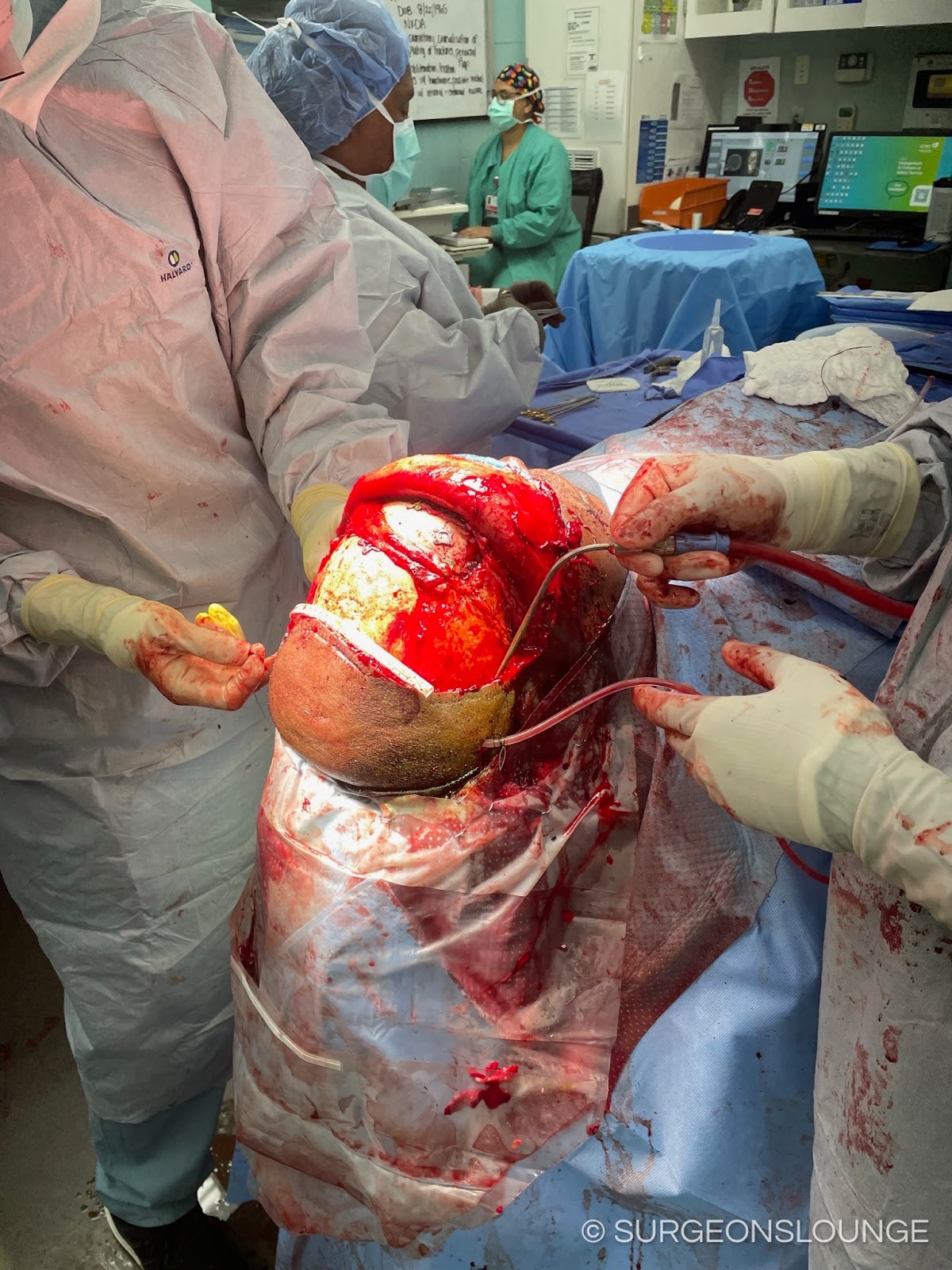
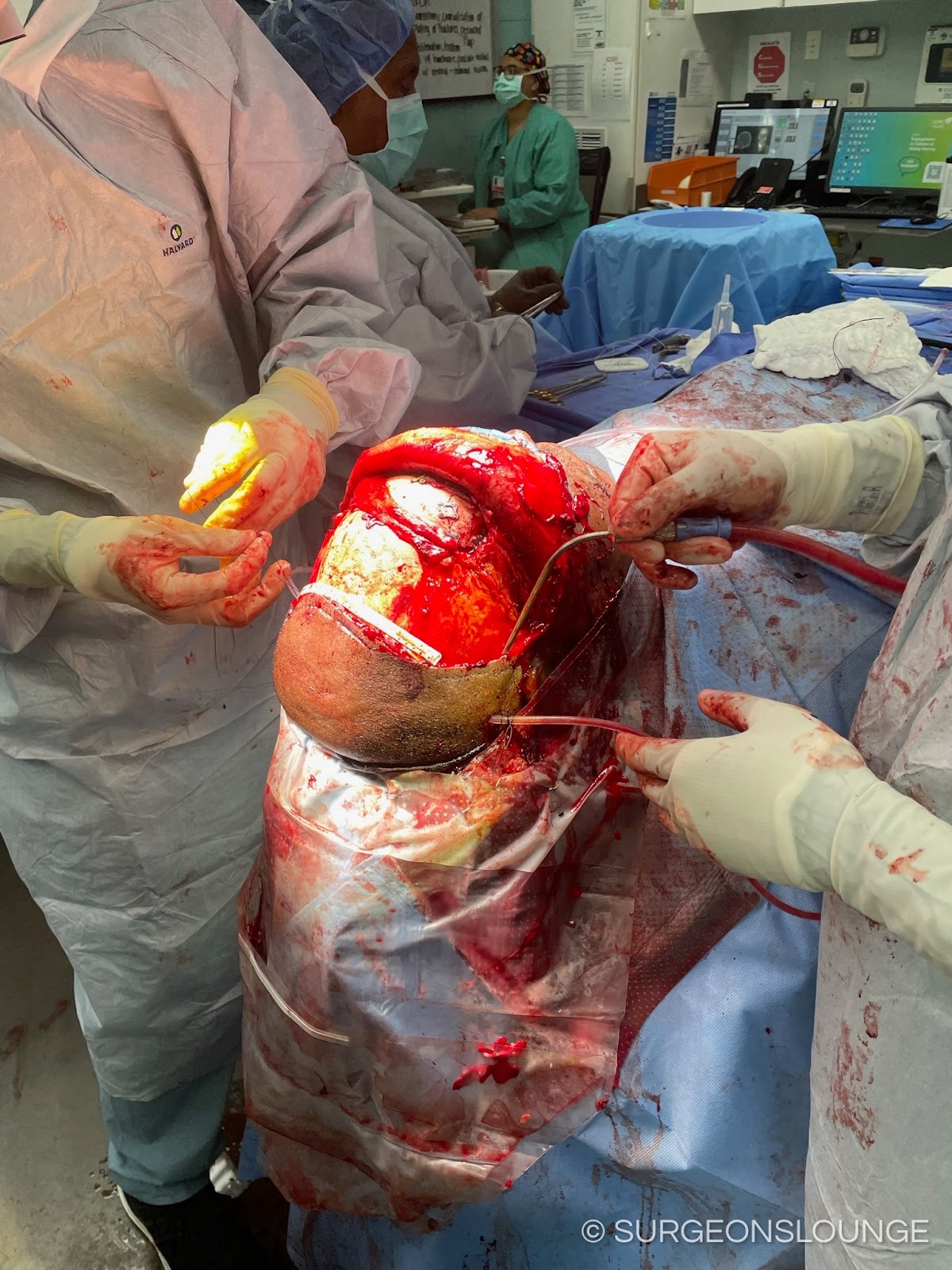
Remove the fractured segments of the anterior table. If necessary, adapt a mesh to the contour of the defect segment. Gently curette the frontal sinus lining. Irrigate the site with copious normal saline irrigation. The frontal sinus can be obliterated with autogenous fat, pericranium, or hydroxyapatite cement. The anterior frontal sinus table can then be reapproximated (or mesh) and fixated with mono cortical fixation.
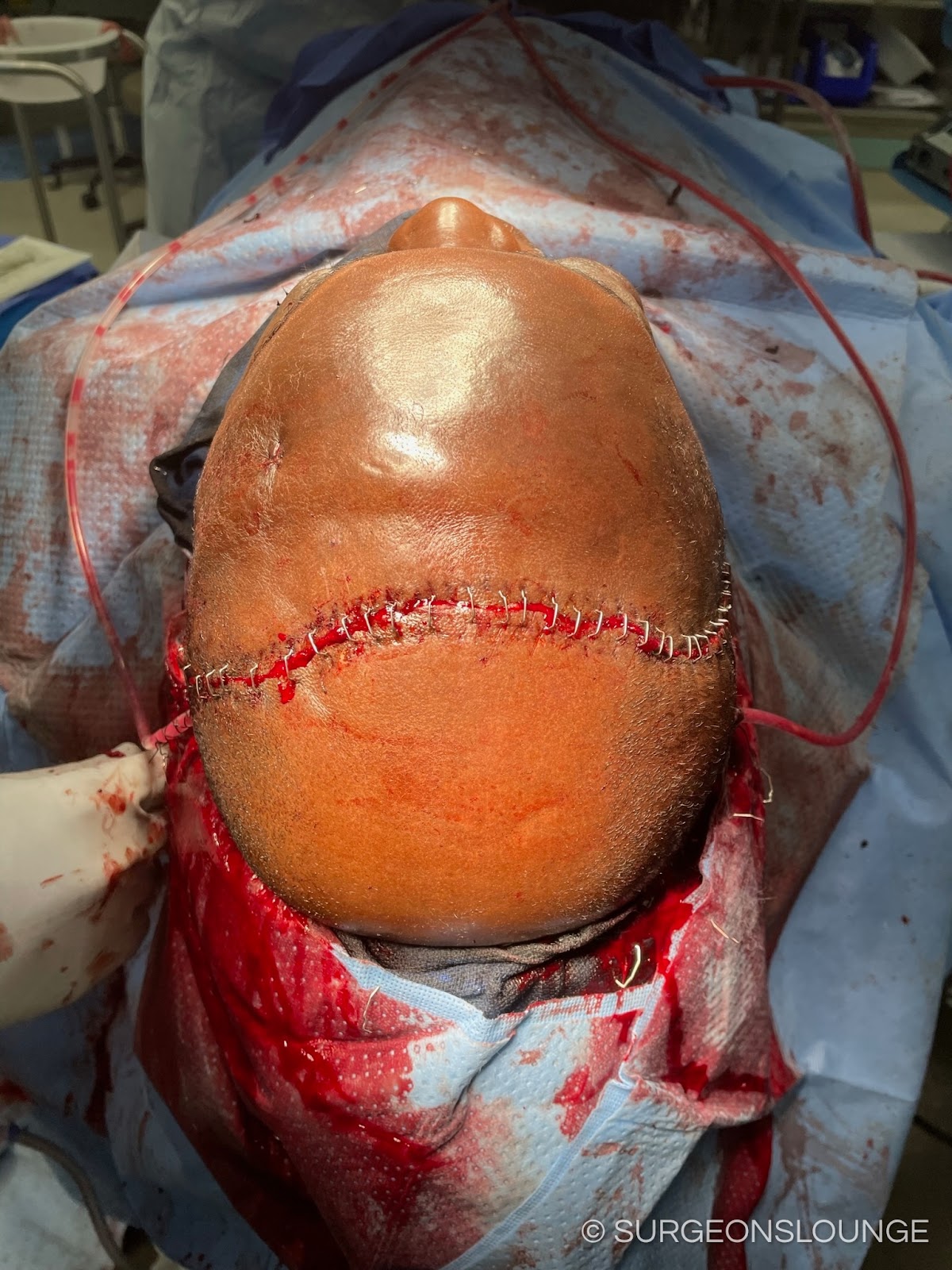
The surgical site was then copously irrigated. Raney clips removed. The surgical site was confirmed to be hemostatic. A flat cranial drain was then placed. The deeper layers of the incision site was then reapproximated and closed with 2-0 vicryl pops. The superficia sin was the reapproximated with a skin stapler. The bulb suction was confirmed to be holding suction. Bacitracin was then used at the incision site and tellfa dressing placed over the incision site.
The patient's face was then cleaned and the posterior pharynx was suctioned. An OG tube was used to suction out the contents of the stomach. Tegaderms were removed from the eyes. Dressings were placed. The patient was then transferred back to the care of the anesthesia team for extubation and recovery.
Coding
- Cpt 21344: ORIF frontal sinus with multiple approches, coronal complicated
- Cpt 31085: Frontal sinus cranialization